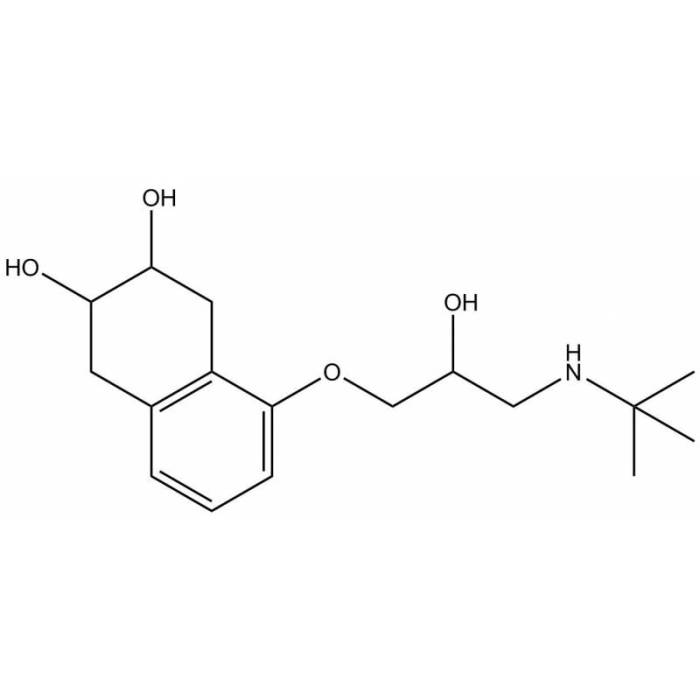
Nadolol, a non-selective beta-blocker, stands as a potent medication commonly prescribed for managing hypertension and angina pectoris. Its mechanism of action revolves around blocking the effects of adrenaline and noradrenaline, hormones that trigger the heart to beat faster and blood vessels to constrict. This blocking action leads to a decrease in blood pressure and heart rate, offering relief from the symptoms of these conditions.
Nadolol is available in various forms, including tablets and oral solutions, providing flexibility in dosage and administration. Its pharmacokinetic profile reveals that it is well absorbed orally, reaching peak blood levels within 2-4 hours. The drug undergoes extensive metabolism in the liver and is excreted primarily in urine.
Contraindications and Precautions
Nadolol, a non-selective beta-blocker, is a medication used to treat high blood pressure, angina, and other cardiovascular conditions. While generally safe and effective, certain situations require careful consideration before initiating nadolol therapy. This section delves into the absolute contraindications to nadolol therapy and Artikels the precautions that should be taken when prescribing this medication.
Absolute Contraindications
Absolute contraindications represent situations where the risk of using nadolol outweighs any potential benefit. In these cases, nadolol should never be used.
- Severe bradycardia: Nadolol slows the heart rate, and in patients with already slow heart rates, it can further decrease the heart rate to dangerous levels, leading to potentially life-threatening complications.
- Second- or third-degree atrioventricular block (AV block): Nadolol can worsen AV block, a condition that disrupts the electrical conduction in the heart, potentially leading to bradycardia and heart failure.
- Sick sinus syndrome: This condition involves a malfunction of the heart’s natural pacemaker, and nadolol can further disrupt the heart’s rhythm, potentially causing bradycardia or heart block.
- Cardiogenic shock: Nadolol can worsen the condition of cardiogenic shock, a life-threatening condition where the heart cannot pump enough blood to meet the body’s needs.
- Uncontrolled heart failure: While nadolol can be used in some patients with heart failure, it is contraindicated in those with uncontrolled heart failure, as it can worsen the condition.
- Hypersensitivity to nadolol or any of its components: Patients with a history of allergic reactions to nadolol or its ingredients should avoid using this medication.
- Pheochromocytoma: This rare tumor of the adrenal glands can release excessive amounts of catecholamines, and nadolol can worsen the symptoms of pheochromocytoma by blocking the beta-adrenergic receptors.
Precautions, Nadolol
While not absolute contraindications, certain conditions and situations warrant caution when prescribing nadolol. Careful monitoring and adjustments in dosage or treatment plan may be necessary.
- Asthma and other respiratory conditions: Nadolol can worsen bronchospasm, a condition that narrows the airways, making it difficult to breathe. Patients with asthma or other respiratory conditions should be carefully monitored for any signs of bronchospasm, and alternative medications may be considered.
- Peripheral vascular disease: Nadolol can exacerbate symptoms of peripheral vascular disease, a condition that affects blood flow to the limbs, by further constricting blood vessels.
- Diabetes: Nadolol can mask the symptoms of hypoglycemia (low blood sugar), potentially leading to serious complications. Patients with diabetes should be carefully monitored for hypoglycemia, and their diabetic medications may need to be adjusted.
- Thyroid disease: Nadolol can mask the symptoms of hyperthyroidism (overactive thyroid), potentially leading to serious complications. Patients with thyroid disease should be carefully monitored for hyperthyroidism, and their thyroid medications may need to be adjusted.
- Renal impairment: Nadolol is eliminated by the kidneys, and in patients with impaired kidney function, the medication may accumulate in the body, increasing the risk of side effects.
- Hepatic impairment: Nadolol is metabolized by the liver, and in patients with impaired liver function, the medication may accumulate in the body, increasing the risk of side effects.
- Pregnancy and lactation: Nadolol can cross the placenta and enter breast milk. While the safety of nadolol during pregnancy and lactation has not been established, it is generally recommended to avoid using nadolol during these periods.
- Elderly patients: Elderly patients are more susceptible to the side effects of nadolol, and lower doses may be necessary.
- Patients undergoing surgery: Nadolol can interfere with the body’s response to anesthesia. Patients undergoing surgery should inform their surgeon about their nadolol use.
Nadolol in Specific Populations
Nadolol, like other medications, requires careful consideration when used in specific populations, such as pregnant women, breastfeeding mothers, pediatric patients, and individuals with renal or hepatic impairment.
Pregnancy and Breastfeeding
Nadolol crosses the placenta and is found in breast milk. It is categorized as a Pregnancy Category C drug, meaning that animal studies have shown adverse effects on the fetus, but there are no adequate and well-controlled studies in pregnant women. The potential risks to the fetus should be weighed against the potential benefits to the mother.
- Pregnancy: Nadolol should be used during pregnancy only if the potential benefits outweigh the potential risks to the fetus. The drug may cause fetal bradycardia and other adverse effects.
- Breastfeeding: Nadolol is excreted in breast milk, and it is recommended that breastfeeding mothers avoid using nadolol or use alternative medications. If breastfeeding is necessary, the infant should be monitored for signs of bradycardia and other adverse effects.
Pediatric Use
Nadolol is not recommended for use in children, as its safety and efficacy have not been established in this population.
Renal Impairment
Nadolol is primarily eliminated by the kidneys. In patients with renal impairment, the dosage of nadolol may need to be adjusted to prevent the accumulation of the drug in the body.
- Mild to Moderate Renal Impairment: The dosage of nadolol may need to be reduced in patients with mild to moderate renal impairment.
- Severe Renal Impairment: Nadolol should be used with caution in patients with severe renal impairment, and the dosage may need to be further reduced.
Hepatic Impairment
Nadolol is metabolized by the liver. In patients with hepatic impairment, the dosage of nadolol may need to be adjusted to prevent the accumulation of the drug in the body.
- Mild to Moderate Hepatic Impairment: The dosage of nadolol may need to be reduced in patients with mild to moderate hepatic impairment.
- Severe Hepatic Impairment: Nadolol should be used with caution in patients with severe hepatic impairment, and the dosage may need to be further reduced.
Nadolol in Research and Development
Nadolol, a beta-blocker commonly used to treat high blood pressure and other cardiovascular conditions, has been the subject of ongoing research exploring its potential applications beyond its traditional therapeutic uses. These investigations aim to identify new avenues for nadolol’s therapeutic benefit, potentially leading to innovative treatment strategies for a wider range of conditions.
Current Research Exploring Potential Applications of Nadolol
Research efforts are underway to investigate the potential of nadolol in various therapeutic areas, such as:
- Neurological disorders: Studies are exploring nadolol’s potential in treating conditions like essential tremor, a neurological disorder causing involuntary shaking, and Parkinson’s disease, a progressive neurodegenerative disorder.
- Cancer: Research is investigating nadolol’s potential role in inhibiting the growth and spread of certain types of cancer, particularly those associated with the beta-adrenergic signaling pathway.
- Migraines: Some studies suggest that nadolol might be effective in preventing migraine headaches, particularly those associated with cardiovascular risk factors.
- Other conditions: Ongoing research is exploring nadolol’s potential in treating conditions like anxiety, hyperthyroidism, and even certain types of glaucoma.
Ongoing Clinical Trials Involving Nadolol
Several clinical trials are currently underway to evaluate the safety and efficacy of nadolol in various therapeutic settings. These trials are investigating the use of nadolol in:
- Essential tremor: Clinical trials are evaluating the effectiveness of nadolol in reducing tremor severity and improving the quality of life in patients with essential tremor.
- Parkinson’s disease: Ongoing clinical trials are exploring nadolol’s potential in managing the motor symptoms associated with Parkinson’s disease, such as tremor, rigidity, and bradykinesia.
- Cancer: Clinical trials are investigating the use of nadolol in combination with other cancer therapies to enhance treatment efficacy and improve patient outcomes.
Future Directions for Research Related to Nadolol
Future research on nadolol will likely focus on:
- Investigating the mechanisms of action: Further research is needed to elucidate the precise mechanisms by which nadolol exerts its therapeutic effects in different conditions, particularly in areas beyond its traditional uses.
- Optimizing dosage and treatment regimens: Studies are likely to explore optimal dosage and treatment regimens for nadolol in different patient populations and for various conditions.
- Developing novel formulations: Research may focus on developing novel formulations of nadolol, such as extended-release or targeted delivery systems, to improve its efficacy and reduce side effects.
- Exploring combination therapies: Future research might investigate the potential benefits of combining nadolol with other medications or therapeutic approaches to enhance treatment outcomes.
Nadolol: A Comparative Perspective
Nadolol, a nonselective beta-blocker, holds a distinct position within the class due to its unique pharmacokinetic profile and clinical applications. Understanding its advantages and disadvantages in comparison to other beta-blockers is crucial for optimizing patient care.
Comparison of Nadolol with Other Beta-Blockers
This section provides a comparative analysis of nadolol against other commonly used beta-blockers, focusing on their efficacy, safety, and pharmacokinetic properties.
- Efficacy: Nadolol is generally considered effective in managing hypertension and other cardiovascular conditions, such as angina and arrhythmias. However, its long half-life may necessitate dose adjustments, particularly in patients with renal impairment. Other beta-blockers, such as metoprolol and atenolol, may offer more flexibility in dosage adjustments.
- Safety: Nadolol, like other beta-blockers, can cause adverse effects such as bradycardia, fatigue, and bronchospasm. However, its long half-life may contribute to a more sustained and predictable effect, reducing the risk of rebound hypertension.
- Pharmacokinetic Properties: Nadolol’s primary advantage lies in its extended half-life, ranging from 10 to 24 hours, allowing for once-daily dosing. This simplifies medication adherence for patients. However, its long half-life also necessitates careful dose titration and monitoring, especially in patients with renal impairment.
Advantages and Disadvantages of Nadolol
Nadolol’s unique pharmacokinetic properties present both advantages and disadvantages compared to other beta-blockers.
Advantages
- Once-daily dosing: Nadolol’s long half-life allows for convenient once-daily administration, improving patient adherence to therapy.
- Sustained effect: The extended duration of action can provide a more consistent and predictable blood pressure control, potentially reducing the risk of rebound hypertension.
Disadvantages
- Limited dosage flexibility: Dose adjustments may be challenging due to the long half-life, especially in patients with renal impairment.
- Potential for drug interactions: Nadolol’s long half-life can increase the risk of drug interactions, requiring careful monitoring of co-administered medications.
Key Differences Between Nadolol and Other Beta-Blockers
The following table summarizes the key differences between nadolol and other commonly used beta-blockers.
| Property | Nadolol | Metoprolol | Atenolol | Propranolol |
|---|---|---|---|---|
| Half-life | 10-24 hours | 3-7 hours | 6-9 hours | 3-6 hours |
| Dosage frequency | Once daily | Twice daily | Once daily | Twice daily |
| Selectivity | Nonselective | Selective (β1) | Selective (β1) | Nonselective |
| Lipid solubility | Low | Moderate | Low | High |
| Clinical applications | Hypertension, angina, arrhythmias | Hypertension, angina, heart failure | Hypertension, angina | Hypertension, angina, migraine prophylaxis |
Nadolol remains a valuable therapeutic option for managing hypertension and angina pectoris, offering a safe and effective approach for many patients. While it is generally well-tolerated, potential adverse effects should be carefully considered. Understanding the drug’s pharmacokinetic profile, interactions, and contraindications is crucial for optimizing patient outcomes. Nadolol’s future research holds promise in exploring its potential applications in other areas of medicine, further solidifying its role in the therapeutic landscape.
Nadolol is a beta-blocker medication used to treat high blood pressure and other cardiovascular conditions. While it’s effective for its intended purpose, it’s important to note that nadolol can interact with certain medications, including pain relievers like darvocet. Therefore, it’s crucial to consult with your doctor about any potential interactions before taking nadolol or any other medications.