Fosinopril, a well-known angiotensin-converting enzyme (ACE) inhibitor, plays a crucial role in managing high blood pressure and other cardiovascular conditions. This medication works by blocking the conversion of angiotensin I to angiotensin II, a powerful vasoconstrictor that elevates blood pressure. By inhibiting this process, fosinopril helps relax blood vessels, reducing pressure on the heart and promoting healthy blood flow.
Fosinopril’s impact extends beyond hypertension, finding application in the treatment of heart failure and diabetic nephropathy. It has proven effective in managing these conditions by mitigating the detrimental effects of angiotensin II on the cardiovascular system and kidneys.
Fosinopril
Fosinopril is a medication that belongs to a class of drugs known as angiotensin-converting enzyme (ACE) inhibitors. It is primarily prescribed to treat high blood pressure (hypertension) and heart failure. Fosinopril works by blocking the action of an enzyme called angiotensin-converting enzyme, which is responsible for converting angiotensin I to angiotensin II. Angiotensin II is a potent vasoconstrictor, meaning it narrows blood vessels, leading to increased blood pressure. By inhibiting this conversion, fosinopril helps to relax blood vessels, lowering blood pressure and reducing the strain on the heart.
Chemical Structure and Molecular Formula
Fosinopril is a synthetic drug with a complex chemical structure. Its molecular formula is C20H31N3O6S. The molecule contains a central core structure consisting of a proline ring attached to a side chain with a sulfhydryl group (-SH). This sulfhydryl group is crucial for the drug’s ability to inhibit ACE. The molecular weight of fosinopril is 441.54 g/mol.
Angiotensin-Converting Enzyme (ACE) Inhibition
ACE inhibitors, such as fosinopril, work by blocking the activity of the angiotensin-converting enzyme (ACE). ACE is an enzyme found in the body that plays a crucial role in regulating blood pressure. When ACE is inhibited, the conversion of angiotensin I to angiotensin II is blocked, leading to a decrease in blood pressure.
Mechanism of Action
Fosinopril is an angiotensin-converting enzyme (ACE) inhibitor that works by blocking the conversion of angiotensin I to angiotensin II. This mechanism of action plays a crucial role in regulating blood pressure and overall cardiovascular health.
Angiotensin II and Blood Pressure Regulation
Angiotensin II is a potent vasoconstrictor, meaning it narrows blood vessels, leading to increased blood pressure. It also stimulates the release of aldosterone, a hormone that promotes sodium and water retention, further contributing to increased blood pressure.
Physiological Effects of Inhibiting Angiotensin II Production
By inhibiting the conversion of angiotensin I to angiotensin II, fosinopril reduces the levels of angiotensin II in the body. This leads to several physiological effects:
- Vasodilation: The reduction in angiotensin II levels allows blood vessels to relax and widen, decreasing peripheral resistance and lowering blood pressure.
- Reduced Aldosterone Release: With lower angiotensin II levels, the release of aldosterone is also reduced. This leads to increased sodium and water excretion, further contributing to lower blood pressure.
- Improved Cardiac Function: By reducing afterload (the pressure the heart has to pump against), fosinopril improves cardiac function, particularly in individuals with heart failure.
Therapeutic Uses
Fosinopril is a medication primarily used to manage high blood pressure (hypertension) and to treat heart failure and diabetic nephropathy. It belongs to a class of drugs known as angiotensin-converting enzyme (ACE) inhibitors, which work by blocking the conversion of angiotensin I to angiotensin II. Angiotensin II is a potent vasoconstrictor that causes blood vessels to narrow, leading to increased blood pressure. By inhibiting this conversion, fosinopril helps to relax blood vessels, reduce blood pressure, and improve blood flow.
Management of Hypertension
Fosinopril is commonly prescribed for the treatment of hypertension. It effectively lowers blood pressure by relaxing blood vessels, allowing blood to flow more easily. When used as directed, fosinopril can help prevent serious health complications associated with high blood pressure, such as stroke, heart attack, and kidney failure.
Treatment of Heart Failure
Fosinopril is also used to treat heart failure. In heart failure, the heart is unable to pump blood effectively, leading to fluid buildup in the body. Fosinopril helps to improve the heart’s pumping function by reducing the workload on the heart and decreasing the amount of fluid in the body.
Treatment of Diabetic Nephropathy
Diabetic nephropathy is a serious complication of diabetes that damages the kidneys. Fosinopril is used to slow the progression of diabetic nephropathy by protecting the kidneys from further damage.
Dosage and Administration
Fosinopril is typically administered orally, with dosage tailored to the individual patient’s needs and medical history. The standard dosage recommendations for fosinopril vary depending on the specific condition being treated.
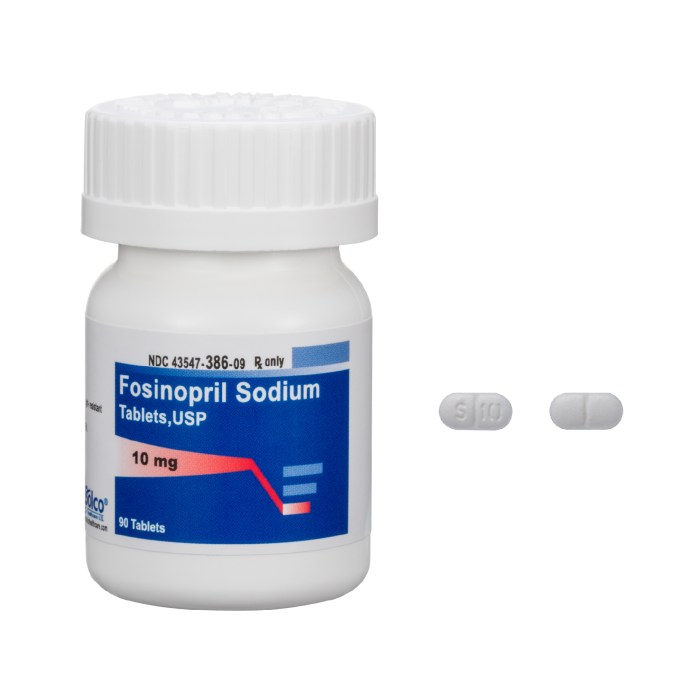
Dosage Forms
Fosinopril is available in tablet form, typically containing 10 mg, 20 mg, or 40 mg of the active ingredient. These tablets are usually taken once daily, with or without food.
Frequency and Duration of Treatment
The frequency and duration of fosinopril treatment are determined by the treating physician and depend on the patient’s individual condition and response to therapy.
Adverse Effects
Like most medications, fosinopril can cause side effects, some common and others more serious. Understanding these potential effects is crucial for safe and effective use.
Common Side Effects
Common side effects of fosinopril are generally mild and often resolve on their own.
- Headache: A common side effect that may be due to changes in blood pressure.
- Dizziness: May be caused by a drop in blood pressure, particularly when standing up quickly.
- Fatigue: Can be a side effect, especially during the initial stages of treatment.
- Cough: A dry, persistent cough can occur in some individuals, and is often related to the medication’s effect on the lungs.
- Gastrointestinal upset: This may include nausea, vomiting, diarrhea, or constipation.
- Skin rash: A mild skin rash can occur in some cases.
Serious Side Effects
While less common, some serious side effects can occur with fosinopril. It’s essential to seek immediate medical attention if you experience any of the following:
- Hypotension: A significant drop in blood pressure can lead to dizziness, lightheadedness, fainting, and even shock. It is particularly important to monitor blood pressure closely, especially during the initial stages of treatment and when adjusting the dosage.
- Angioedema: A rare but serious allergic reaction that can cause swelling of the face, lips, tongue, and throat. This swelling can obstruct breathing and require immediate medical attention.
- Hyperkalemia: An elevation of potassium levels in the blood can be dangerous, especially for individuals with pre-existing kidney problems. Regular monitoring of potassium levels is important, particularly for those at risk.
- Renal impairment: Fosinopril can worsen kidney function in some individuals, especially those with pre-existing kidney disease. Regular monitoring of kidney function is essential.
Hypotension
Hypotension, or low blood pressure, is a common side effect of fosinopril, particularly during the initial stages of treatment. It is often associated with dizziness, lightheadedness, and fainting.
It is crucial to monitor blood pressure closely, especially during the initial stages of treatment and when adjusting the dosage.
To minimize the risk of hypotension, healthcare providers often recommend starting with a low dose of fosinopril and gradually increasing it as needed.
Cough, Fosinopril
A dry, persistent cough is a relatively common side effect of fosinopril, affecting about 10-20% of individuals taking the medication.
This cough is thought to be caused by the medication’s effect on the lungs, specifically by increasing the production of bradykinin, a substance that can trigger coughing.
If the cough becomes bothersome or interferes with daily activities, it’s important to discuss it with your healthcare provider. They may recommend alternative medications or dosage adjustments.
Angioedema
Angioedema is a rare but serious allergic reaction that can occur with fosinopril. It is characterized by rapid swelling of the face, lips, tongue, and throat.
This swelling can obstruct breathing and require immediate medical attention.
If you experience any swelling, particularly around the face or throat, seek immediate medical attention.
Monitoring for Adverse Reactions
It is essential to monitor for adverse reactions to fosinopril. This involves regular blood pressure checks, particularly during the initial stages of treatment and when adjusting the dosage. Additionally, it is important to be aware of any unusual symptoms or changes in your health and to report them to your healthcare provider.
Contraindications and Precautions
Fosinopril, like other ACE inhibitors, has specific contraindications and precautions that healthcare professionals should be aware of to ensure patient safety and optimize treatment outcomes.
Contraindications
- History of angioedema associated with ACE inhibitor use: Previous exposure to ACE inhibitors can lead to angioedema, a potentially life-threatening condition characterized by swelling of the face, lips, tongue, and throat. Fosinopril is contraindicated in patients with a history of angioedema related to ACE inhibitor use.
- Hereditary or idiopathic angioedema: Patients with hereditary or idiopathic angioedema are at an increased risk of developing angioedema with ACE inhibitors.
- Second and third trimester of pregnancy: Fosinopril can cause fetal harm, including fetal death, if used during the second and third trimesters of pregnancy. It is contraindicated in these stages.
Precautions
- Hypersensitivity to fosinopril or other ACE inhibitors: Patients with known hypersensitivity to fosinopril or other ACE inhibitors should avoid using the drug.
- Renal impairment: Fosinopril is excreted primarily by the kidneys. In patients with impaired renal function, the dosage of fosinopril should be adjusted to prevent accumulation and potential toxicity.
- Hepatic impairment: Fosinopril is metabolized in the liver. In patients with impaired liver function, the dosage of fosinopril may need to be adjusted to prevent accumulation and potential toxicity.
- Electrolyte disturbances: ACE inhibitors can cause electrolyte disturbances, such as hypokalemia (low potassium levels) and hyperkalemia (high potassium levels). Patients with pre-existing electrolyte imbalances should be monitored closely.
- Diabetes: Fosinopril can enhance the effects of insulin and other antidiabetic medications. Patients with diabetes should be closely monitored for hypoglycemia (low blood sugar).
- Surgery/anesthesia: Fosinopril can interact with certain anesthetics, potentially causing hypotension (low blood pressure). It is important to inform the anesthesiologist about fosinopril use before surgery.
- Collagen vascular diseases: Patients with collagen vascular diseases, such as systemic lupus erythematosus (SLE), may be at an increased risk of developing neutropenia (low white blood cell count) while on ACE inhibitors.
- Lithium: Fosinopril can increase lithium levels in the blood. Patients taking lithium should be closely monitored for lithium toxicity.
- Diuretics: Concurrent use of fosinopril and diuretics can increase the risk of hypotension.
- Potassium supplements, potassium-sparing diuretics: These medications can increase potassium levels in the blood, potentially leading to hyperkalemia when used with fosinopril.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs can reduce the effectiveness of fosinopril by interfering with its ability to lower blood pressure.
- Gold: Fosinopril can increase the risk of developing a serious skin reaction (necrotizing vasculitis) in patients receiving gold injections.
Patient Education and Monitoring
- Importance of regular follow-up appointments: Patients should be advised to attend regular follow-up appointments to monitor blood pressure, kidney function, and electrolyte levels.
- Early recognition and reporting of side effects: Patients should be educated about potential side effects of fosinopril, such as cough, dizziness, and angioedema. They should be instructed to report any unusual symptoms to their healthcare provider immediately.
- Importance of adherence to medication regimen: Patients should be encouraged to take fosinopril as prescribed and to avoid missing doses.
- Lifestyle modifications: Patients should be advised to make lifestyle changes, such as reducing sodium intake, exercising regularly, and maintaining a healthy weight, to help manage hypertension.
Fosinopril vs. Other ACE Inhibitors
Fosinopril is one of several ACE inhibitors available for treating hypertension and other cardiovascular conditions. It is important to understand how fosinopril compares to other ACE inhibitors in terms of its pharmacokinetic profile, therapeutic effects, and overall clinical utility. This comparison will help you determine which ACE inhibitor might be the best option for a given patient.
Pharmacokinetic Profiles of ACE Inhibitors
The pharmacokinetic profile of an ACE inhibitor refers to how the drug is absorbed, distributed, metabolized, and eliminated by the body. Key pharmacokinetic parameters include:
- Absorption: ACE inhibitors are generally well-absorbed from the gastrointestinal tract, but the rate and extent of absorption can vary between different drugs.
- Distribution: ACE inhibitors are widely distributed throughout the body, including the heart, blood vessels, and kidneys.
- Metabolism: Some ACE inhibitors, such as fosinopril, are prodrugs that are metabolized in the body to form the active drug. Others, like lisinopril, are active drugs that are not metabolized.
- Elimination: ACE inhibitors are primarily eliminated through the kidneys. The elimination half-life, which is the time it takes for the drug concentration in the body to decrease by half, can vary between different drugs.
Fosinopril, for example, is a prodrug that is metabolized in the body to form the active drug, fosinoprilat. Fosinopril has a relatively long half-life of about 12 hours, while lisinopril has a shorter half-life of about 11 hours. This means that fosinopril may need to be administered less frequently than lisinopril to achieve a similar therapeutic effect.
Therapeutic Effects of ACE Inhibitors
ACE inhibitors are primarily used to treat hypertension and heart failure. They work by blocking the activity of the angiotensin-converting enzyme (ACE), which is involved in the production of angiotensin II. Angiotensin II is a potent vasoconstrictor that raises blood pressure. By blocking ACE, ACE inhibitors prevent the formation of angiotensin II, leading to vasodilation and a decrease in blood pressure.
Rationale for Choosing One ACE Inhibitor over Another
The choice of ACE inhibitor often depends on several factors, including:
- Patient’s clinical condition: The severity of hypertension, the presence of other cardiovascular conditions, and the patient’s overall health status are important considerations.
- Pharmacokinetic profile: The absorption, distribution, metabolism, and elimination characteristics of the ACE inhibitor can influence the dosing regimen and the risk of adverse effects.
- Drug interactions: Some ACE inhibitors may interact with other medications, so it is important to consider the patient’s current medication regimen.
- Cost: The cost of the ACE inhibitor can also be a factor in the decision-making process.
For example, if a patient has severe hypertension and needs a long-acting ACE inhibitor, fosinopril with its longer half-life might be a good option. However, if a patient has kidney problems, lisinopril might be a better choice because it is primarily eliminated through the kidneys.
Research and Development
Fosinopril, like many other medications, underwent a rigorous research and development process to ensure its safety and efficacy before being made available to patients. This process involved multiple stages, including preclinical studies, clinical trials, and ongoing research to further understand its effects and potential applications.
The development of fosinopril began in the 1970s with the discovery of the angiotensin-converting enzyme (ACE) and its role in regulating blood pressure. Researchers at the pharmaceutical company Merck & Co. Inc. identified a compound that inhibited ACE, leading to the development of the first ACE inhibitor, captopril. This success paved the way for the development of other ACE inhibitors, including fosinopril.
Clinical Trials
Clinical trials are crucial for evaluating the safety and efficacy of new drugs. Fosinopril underwent extensive clinical trials to assess its effectiveness in treating hypertension and its potential side effects.
The first clinical trials of fosinopril began in the early 1980s. These trials involved patients with hypertension and aimed to determine the optimal dosage, safety profile, and efficacy of fosinopril compared to existing treatments.
The results of these trials demonstrated that fosinopril effectively lowered blood pressure in patients with hypertension. It was also found to be well-tolerated, with a similar safety profile to other ACE inhibitors.
These clinical trials were pivotal in establishing the safety and efficacy of fosinopril, leading to its approval by regulatory agencies for the treatment of hypertension.
Ongoing Research
While fosinopril has been available for decades, research continues to explore its potential applications and investigate its long-term effects.
One area of ongoing research focuses on the use of fosinopril in the treatment of heart failure. Clinical trials have shown that fosinopril can improve symptoms and reduce the risk of death in patients with heart failure.
Another area of interest is the potential role of fosinopril in preventing kidney disease. Studies suggest that fosinopril may slow the progression of kidney damage in patients with diabetes or other conditions that affect the kidneys.
Ongoing research also investigates the long-term safety of fosinopril, including its effects on bone health and the risk of developing cancer.
These ongoing research efforts aim to expand our understanding of fosinopril’s benefits and risks, potentially leading to new applications and improved patient care.
Patient Information: Fosinopril

Fosinopril is a medication that helps lower blood pressure. It is used to treat high blood pressure and heart failure. This information sheet will help you understand what fosinopril is, how it works, and what you need to know before taking it.
Key Information About Fosinopril
This table summarizes important information about fosinopril:
| Information | Details |
|---|---|
| What it is used for | Fosinopril is used to treat high blood pressure and heart failure. It helps lower blood pressure and makes it easier for the heart to pump blood. |
| How to take it | Fosinopril is usually taken once a day, with or without food. You should swallow the tablet whole, with a glass of water. Do not crush or chew the tablet. Your doctor will tell you how much to take and how often. |
| Potential side effects | Like all medicines, fosinopril can cause side effects, but not everyone gets them. Some common side effects include:
In rare cases, fosinopril can cause more serious side effects. If you experience any of the following, stop taking fosinopril and contact your doctor immediately:
|
| Important precautions | Before taking fosinopril, tell your doctor if you:
It is important to take fosinopril exactly as prescribed by your doctor. Do not stop taking fosinopril without talking to your doctor first. |
Patient Information Leaflet
This leaflet provides information for patients about fosinopril. It is not a substitute for talking to your doctor or pharmacist.
What is Fosinopril?
Fosinopril is a medicine that helps lower blood pressure. It belongs to a group of medicines called angiotensin-converting enzyme (ACE) inhibitors. Fosinopril works by relaxing blood vessels, which makes it easier for blood to flow through them. This lowers blood pressure.
Why am I taking Fosinopril?
You are taking fosinopril to treat high blood pressure or heart failure. High blood pressure can damage your heart, blood vessels, kidneys, and eyes. Heart failure is a condition where your heart is not able to pump blood around your body properly. Fosinopril helps to reduce these risks by lowering your blood pressure and making it easier for your heart to pump blood.
How do I take Fosinopril?
Your doctor will tell you how much fosinopril to take and how often. You should take fosinopril once a day, with or without food. Swallow the tablet whole, with a glass of water. Do not crush or chew the tablet.
What if I miss a dose?
If you miss a dose of fosinopril, take it as soon as you remember. However, if it is almost time for your next dose, skip the missed dose and take your next dose at the usual time. Do not take a double dose to make up for a missed dose.
What if I take too much Fosinopril?
If you take too much fosinopril, contact your doctor or local poison control center immediately.
What are the possible side effects of Fosinopril?
Like all medicines, fosinopril can cause side effects, but not everyone gets them. Some common side effects include:
- Cough
- Dizziness
- Headache
In rare cases, fosinopril can cause more serious side effects. If you experience any of the following, stop taking fosinopril and contact your doctor immediately:
- Swelling of the face, lips, tongue, or throat
- Difficulty breathing
- Rash
- Yellowing of the skin or eyes
Important information about Fosinopril
Before taking fosinopril, tell your doctor if you:
- Are pregnant or breastfeeding
- Have kidney or liver problems
- Have a history of angioedema
- Are taking any other medications, including over-the-counter medications and herbal supplements
It is important to take fosinopril exactly as prescribed by your doctor. Do not stop taking fosinopril without talking to your doctor first.
How to store Fosinopril
Store fosinopril at room temperature, away from light and moisture. Keep fosinopril out of reach of children.
Where can I get more information?
If you have any questions about fosinopril, talk to your doctor or pharmacist.
Understanding the mechanism of action, therapeutic uses, and potential side effects of fosinopril is essential for both healthcare professionals and patients. This knowledge empowers informed decision-making regarding treatment options and promotes responsible medication use. As with any medication, consulting with a healthcare provider is crucial for personalized guidance and ensuring optimal outcomes.
Fosinopril is a medication used to treat high blood pressure and heart failure. It works by relaxing blood vessels and reducing the amount of fluid in the body. While fosinopril is effective in managing these conditions, it’s important to remember that it’s not a cure-all. For individuals struggling with type 2 diabetes, another medication like jardiance 10 mg may be recommended alongside fosinopril to manage blood sugar levels.
The combination of these medications can be a valuable tool in controlling both blood pressure and blood sugar, contributing to overall health improvement.