Anticoagulant drugs, often referred to as blood thinners, play a crucial role in preventing the formation of potentially life-threatening blood clots. These medications work by interfering with the body’s natural clotting mechanisms, reducing the risk of stroke, heart attack, and pulmonary embolism.
Understanding the different types of anticoagulants, their mechanisms of action, and their appropriate use is essential for healthcare professionals and patients alike. This comprehensive guide delves into the world of anticoagulants, exploring their indications, pharmacokinetics, monitoring, adverse effects, and interactions, along with ethical considerations and historical context.
New Developments in Anticoagulation
The field of anticoagulation has undergone significant advancements in recent years, leading to the development of new drugs with improved efficacy, safety, and convenience. These novel anticoagulants offer several advantages over traditional therapies, including reduced risk of bleeding, improved patient compliance, and a more targeted approach to anticoagulation.
Emerging Anticoagulants and Their Advantages and Disadvantages
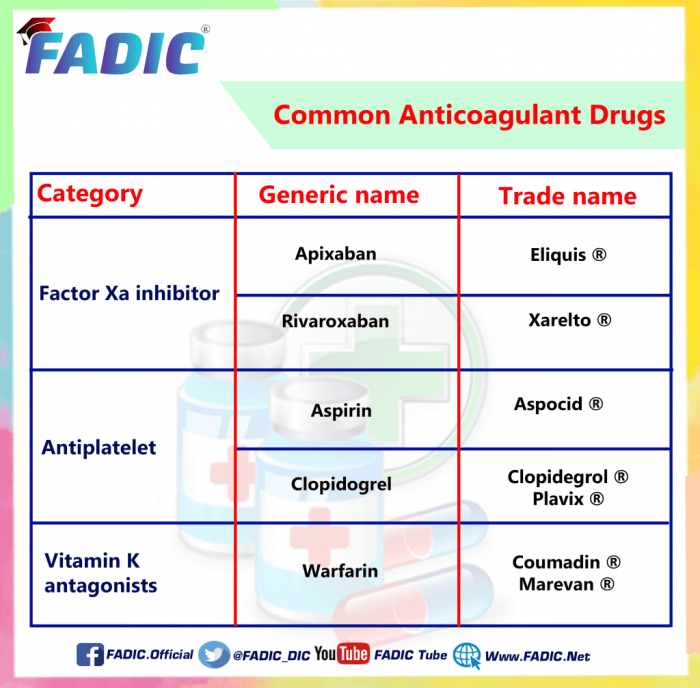
The emergence of new anticoagulants has revolutionized the management of thromboembolic disorders. These agents are classified into two main categories: direct oral anticoagulants (DOACs) and factor Xa inhibitors.
- Direct Oral Anticoagulants (DOACs): DOACs directly inhibit thrombin, a key enzyme in the coagulation cascade. Examples of DOACs include dabigatran, rivaroxaban, apixaban, and edoxaban.
- Advantages: DOACs offer several advantages over traditional anticoagulants, including:
- Reduced risk of bleeding: DOACs have a lower risk of bleeding compared to warfarin, particularly intracranial hemorrhage.
- No need for regular monitoring: Unlike warfarin, DOACs do not require regular INR monitoring, making them more convenient for patients.
- Fixed dosing: DOACs are available in fixed doses, eliminating the need for dose adjustments based on INR levels.
- Improved patient compliance: The convenience and ease of use of DOACs contribute to better patient adherence to therapy.
- Disadvantages:
- Cost: DOACs are generally more expensive than warfarin.
- Limited reversal options: In contrast to warfarin, which can be reversed with vitamin K, there are limited reversal options for DOACs.
- Advantages: DOACs offer several advantages over traditional anticoagulants, including:
- Factor Xa Inhibitors: Factor Xa inhibitors directly block the activity of factor Xa, another crucial enzyme in the coagulation cascade. Examples include rivaroxaban, apixaban, and edoxaban.
- Advantages: Similar to DOACs, factor Xa inhibitors offer several advantages, including:
- Reduced risk of bleeding: Factor Xa inhibitors have a lower risk of bleeding compared to warfarin.
- No need for regular monitoring: Like DOACs, factor Xa inhibitors do not require regular INR monitoring.
- Fixed dosing: Factor Xa inhibitors are available in fixed doses, simplifying administration.
- Improved patient compliance: The convenience of factor Xa inhibitors promotes better patient adherence.
- Disadvantages:
- Cost: Factor Xa inhibitors are generally more expensive than warfarin.
- Limited reversal options: While there are specific reversal agents for some factor Xa inhibitors, such as andexanet alfa for rivaroxaban and apixaban, their availability and effectiveness may vary.
Anticoagulant Therapy in Specific Populations

Anticoagulant therapy in specific populations, such as pregnant women, breastfeeding mothers, children, and individuals with renal or hepatic impairment, requires careful consideration due to unique physiological and pharmacological factors.Anticoagulant Therapy in Pregnancy and Breastfeeding
The use of anticoagulants during pregnancy and breastfeeding is a complex issue that necessitates a careful balance between maternal and fetal well-being.
- Warfarin, a vitamin K antagonist, is contraindicated in pregnancy due to its teratogenic potential, causing fetal bleeding, bone abnormalities, and developmental issues.
- Heparin, a parenteral anticoagulant, is generally considered safe during pregnancy, with minimal placental transfer. However, long-term heparin use can lead to osteoporosis in the mother.
- Low-molecular-weight heparins (LMWHs), such as enoxaparin and dalteparin, are preferred over unfractionated heparin due to their predictable pharmacokinetics and lower risk of bleeding.
- Direct oral anticoagulants (DOACs), such as rivaroxaban, apixaban, and edoxaban, are generally avoided during pregnancy due to limited safety data. However, some studies suggest that these agents may be used with caution in specific circumstances, under close monitoring.
Breastfeeding mothers should consult with their healthcare provider regarding the safety of anticoagulants. While most anticoagulants are excreted in breast milk in small amounts, their impact on infants is generally minimal.
Anticoagulant Therapy in Children, Anticoagulant drugs
Anticoagulant therapy in children presents unique challenges due to their smaller size, evolving physiology, and potential for rapid growth.
- Heparin is the most commonly used anticoagulant in children, with LMWHs gaining popularity due to their convenience and efficacy.
- Warfarin is rarely used in children, due to its teratogenic potential and the difficulty in achieving therapeutic levels in infants and young children.
- DOACs are not approved for use in children under the age of 18, and their safety and efficacy in this population are not fully established.
Anticoagulation dosing in children requires careful adjustment based on age, weight, and specific medical condition. Close monitoring of coagulation parameters is essential to ensure optimal therapeutic effect and minimize the risk of bleeding.
Anticoagulant Therapy in Patients with Renal or Hepatic Impairment
Anticoagulant therapy in patients with renal or hepatic impairment requires special considerations due to the potential for altered drug metabolism and excretion.
- Heparin is generally safe in patients with renal impairment, but may require dose adjustment based on renal function.
- LMWHs are generally safe in patients with mild to moderate renal impairment, but should be used with caution in severe renal impairment.
- Warfarin is contraindicated in patients with severe hepatic impairment, as it is primarily metabolized by the liver.
- DOACs are contraindicated in patients with severe renal impairment, as they are primarily eliminated through the kidneys.
Close monitoring of coagulation parameters is essential in patients with renal or hepatic impairment, to ensure optimal therapeutic effect and minimize the risk of bleeding.
Anticoagulant drugs are essential for preventing blood clots, but they can sometimes interact with other medications. For instance, esmolol , a beta-blocker used to control heart rate, may increase the risk of bleeding when combined with certain anticoagulants. Therefore, it’s crucial to inform your doctor about all medications you’re taking, including over-the-counter drugs and supplements, to ensure safe and effective treatment.
Ethical Considerations in Anticoagulant Therapy: Anticoagulant Drugs
Anticoagulant therapy, while essential for preventing and treating thromboembolic events, raises complex ethical considerations. Balancing the benefits of preventing blood clots with the risks of bleeding and other complications requires careful consideration of the patient’s individual needs and preferences.
Informed Consent and Patient Autonomy
Informed consent is a cornerstone of ethical medical practice. It ensures that patients have the necessary information to make informed decisions about their healthcare. In the context of anticoagulant therapy, informed consent involves discussing the potential benefits and risks of treatment, including the possibility of bleeding complications, with the patient. This process empowers patients to understand their options and make choices that align with their values and preferences.
Potential Conflicts of Interest and Their Management
Conflicts of interest can arise in anticoagulant therapy, particularly when healthcare professionals have financial incentives related to the prescription of specific drugs. These conflicts can undermine the patient’s trust and potentially lead to inappropriate treatment decisions. To mitigate these risks, transparency is crucial. Healthcare professionals should disclose any potential conflicts of interest to their patients, and institutions should have policies in place to manage these conflicts.
Anticoagulants in History
The journey of anticoagulants is a fascinating story of scientific breakthroughs, accidental discoveries, and relentless pursuit of safer and more effective treatments for blood clotting disorders. From ancient remedies to modern-day pharmaceuticals, anticoagulants have played a pivotal role in revolutionizing healthcare, saving countless lives, and improving the quality of life for millions.
Early Discoveries and Traditional Remedies
Long before the advent of modern medicine, ancient civilizations recognized the importance of blood clotting and its implications for health. Egyptians, for instance, used leeches to draw blood, a practice that likely stemmed from the observation that leech saliva contained anticoagulant properties. This practice was documented in ancient Egyptian medical texts, suggesting that the therapeutic potential of anticoagulants was recognized early on. Other traditional remedies included the use of plant extracts like garlic and ginger, which were believed to possess anticoagulant properties. These traditional remedies, while often based on empirical observations, paved the way for the development of modern anticoagulants.
The Dawn of Scientific Understanding
The scientific understanding of blood clotting began to take shape in the 19th century. In 1864, Paul Bert, a French physiologist, discovered that heparin, a substance found in the liver, had anticoagulant properties. Heparin’s discovery was a significant milestone, as it provided the first scientific basis for understanding the mechanism of blood clotting and its inhibition. This discovery led to the development of the first heparin-based anticoagulants, which revolutionized the treatment of thromboembolic disorders.
The Birth of Warfarin
The discovery of warfarin, another widely used anticoagulant, is an interesting tale of serendipity. In the 1940s, researchers at the Wisconsin Alumni Research Foundation (WARF) were investigating the cause of “sweet clover disease,” a condition that affected cattle and caused excessive bleeding. Their research led to the identification of a compound, later named warfarin, which was responsible for the disease. It was soon realized that warfarin had potent anticoagulant properties, and its use in humans was quickly explored. Warfarin became a cornerstone of anticoagulant therapy, offering a safer and more convenient alternative to heparin.
The Era of Oral Anticoagulants
The introduction of oral anticoagulants, such as warfarin, marked a significant shift in the management of thromboembolic disorders. These drugs allowed for convenient and long-term anticoagulation therapy, making it possible for patients to manage their conditions effectively at home. This development revolutionized the treatment of conditions like deep vein thrombosis (DVT), pulmonary embolism (PE), and atrial fibrillation (AFib), reducing the risk of potentially life-threatening complications.
The Quest for Improved Safety and Efficacy
Despite the success of warfarin, its narrow therapeutic window and the need for frequent blood monitoring posed challenges. The quest for safer and more effective anticoagulants continued, leading to the development of newer drugs with improved properties. These newer agents, including dabigatran, rivaroxaban, apixaban, and edoxaban, represent a new generation of anticoagulants that offer several advantages over warfarin, such as a wider therapeutic window, fewer drug interactions, and a reduced need for frequent blood monitoring.
The Future of Anticoagulants
The field of anticoagulant therapy continues to evolve rapidly, driven by ongoing research and technological advancements. Future research focuses on developing novel anticoagulants with even better safety profiles, improved efficacy, and tailored approaches to individual patient needs. The development of personalized medicine and targeted therapies holds immense promise for the future of anticoagulation, offering hope for more effective and individualized treatments.
Anticoagulant therapy has revolutionized the management of thromboembolic disorders, offering patients a lifeline against devastating cardiovascular events. By understanding the complexities of these medications and adhering to prescribed regimens, individuals can effectively manage their condition and live healthier lives.
- Advantages: Similar to DOACs, factor Xa inhibitors offer several advantages, including: