Fluconazole 200 mg stands as a powerful antifungal medication, widely used to combat a range of fungal infections. Its effectiveness stems from its ability to disrupt the growth and development of fungi, making it a valuable tool in treating conditions like yeast infections, ringworm, and athlete’s foot. Fluconazole 200 mg is available in both oral and intravenous forms, offering flexibility in treatment administration. Understanding its mechanism of action, dosage guidelines, potential side effects, and interactions is crucial for safe and effective use.
This comprehensive guide explores the multifaceted nature of fluconazole 200 mg, delving into its chemical structure, medical applications, dosage considerations, potential risks, and the ongoing research surrounding this important antifungal agent.
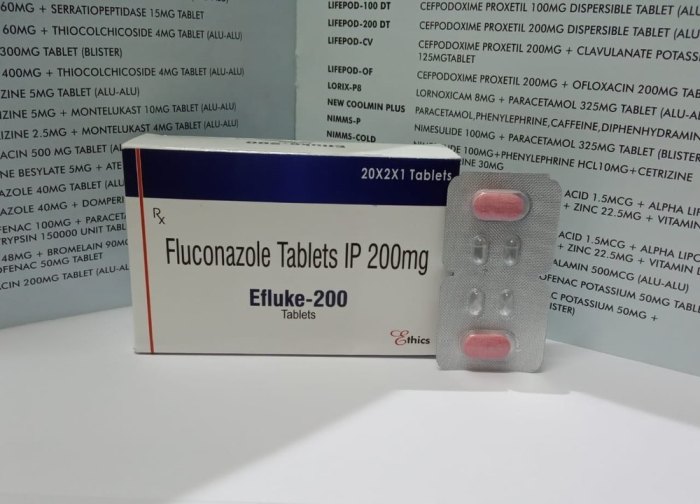
Fluconazole 200 mg
Fluconazole 200 mg is a commonly prescribed antifungal medication used to treat a wide range of fungal infections. It is available in various forms, including oral capsules and intravenous solutions. Fluconazole is a powerful antifungal agent that works by inhibiting the synthesis of ergosterol, a vital component of fungal cell membranes. This disruption leads to the death of fungal cells, effectively treating the infection.
Chemical Structure and Properties
Fluconazole is a synthetic triazole antifungal agent with the chemical name (2R,3S)-2-(2,4-difluorophenyl)-1,3-bis(1H-1,2,4-triazol-1-yl)propan-2-ol. Its molecular formula is C13H12F2N6O and its molecular weight is 306.27 g/mol. Fluconazole is a white to off-white crystalline powder that is practically insoluble in water but soluble in organic solvents like methanol and ethanol.
Pharmaceutical Form and Dosage
Fluconazole 200 mg is available in various pharmaceutical forms, including:
- Oral capsules: These are the most common form of fluconazole and are available in strengths of 50 mg, 100 mg, 150 mg, and 200 mg.
- Oral suspension: This form is suitable for patients who have difficulty swallowing capsules. It is available in a concentration of 40 mg/mL.
- Intravenous solution: This form is administered directly into a vein and is used for patients who cannot take oral medications.
The dosage of fluconazole 200 mg varies depending on the type and severity of the fungal infection being treated. It is typically taken once daily, either with or without food.
Mechanism of Action
Fluconazole 200 mg works by inhibiting the synthesis of ergosterol, a vital component of fungal cell membranes. This inhibition disrupts the integrity of the fungal cell membrane, leading to cell death and the elimination of the infection.
Fluconazole is a selective inhibitor of the fungal enzyme cytochrome P450 14α-demethylase (CYP450 14α-DM), which is responsible for the conversion of lanosterol to ergosterol.
Fluconazole’s high affinity for fungal CYP450 14α-DM, compared to its affinity for human CYP450 enzymes, contributes to its selective antifungal activity.
Medical Uses of Fluconazole 200 mg
Fluconazole 200 mg is a potent antifungal medication that effectively targets a wide range of fungal infections. It belongs to a class of drugs called triazoles, which work by inhibiting the synthesis of ergosterol, a vital component of fungal cell membranes. This disruption in fungal cell structure ultimately leads to the death of the fungus.
Types of Fungal Infections Treated
Fluconazole 200 mg is commonly prescribed for the treatment of various fungal infections, including:
- Candidiasis: This is a common fungal infection caused by the yeast Candida albicans. Fluconazole is effective in treating various types of candidiasis, including oral thrush, vaginal yeast infections, and esophageal candidiasis.
- Cryptococcosis: This is a serious fungal infection caused by the fungus Cryptococcus neoformans. Fluconazole is used to treat both cryptococcal meningitis and cryptococcal pneumonia.
- Coccidioidomycosis: This is a fungal infection caused by the fungus Coccidioides immitis. Fluconazole is used to treat both mild and severe cases of coccidioidomycosis.
- Blastomycosis: This is a fungal infection caused by the fungus Blastomyces dermatitidis. Fluconazole is used to treat both pulmonary and extrapulmonary blastomycosis.
- Histoplasmosis: This is a fungal infection caused by the fungus Histoplasma capsulatum. Fluconazole is used to treat both acute and chronic histoplasmosis.
Common Indications for Prescribing
Fluconazole 200 mg is commonly prescribed for the following reasons:
- Treatment of fungal infections: As mentioned above, fluconazole is effective in treating a wide range of fungal infections.
- Prophylaxis of fungal infections: Fluconazole can also be used to prevent fungal infections in patients who are at high risk, such as those with weakened immune systems or those undergoing certain medical procedures.
- Treatment of fungal infections in specific patient populations: Fluconazole is often used to treat fungal infections in patients with certain medical conditions, such as HIV/AIDS, cancer, or organ transplantation.
Specific Uses in Different Patient Populations
Fluconazole 200 mg is used to treat fungal infections in a variety of patient populations, including:
- Children: Fluconazole is safe and effective for treating fungal infections in children, but the dosage must be adjusted based on the child’s weight and age.
- Pregnant women: Fluconazole is considered safe for use during pregnancy, but it should only be used if the potential benefits outweigh the potential risks.
- Breastfeeding women: Fluconazole is excreted in breast milk, so it should be used with caution in breastfeeding women.
- Elderly patients: Fluconazole may be used in elderly patients, but the dosage may need to be adjusted due to age-related changes in kidney function.
Dosage and Administration of Fluconazole 200 mg
Fluconazole 200 mg is available in oral and intravenous forms. The dosage and frequency of administration vary depending on the type of fungal infection being treated, the patient’s age, weight, and kidney function. It’s crucial to consult with a healthcare professional to determine the appropriate dosage and administration for your specific needs.
Oral Administration
Oral fluconazole is typically taken once daily with or without food. The dosage and duration of treatment depend on the specific fungal infection being treated.
- Dosage: The usual adult dose for most fungal infections is 100-400 mg daily. The dosage may be adjusted based on the severity of the infection and the patient’s response to treatment.
- Frequency: The medication is typically taken once daily.
- Duration: The duration of treatment varies depending on the type of fungal infection being treated. For example, treatment for vaginal candidiasis may last 1-3 days, while treatment for cryptococcal meningitis may last several weeks or months.
Intravenous Administration
Intravenous fluconazole is used when oral administration is not possible or when a higher concentration of the drug is needed.
- Dosage: The usual adult dose for most fungal infections is 400 mg daily. The dosage may be adjusted based on the severity of the infection and the patient’s response to treatment.
- Frequency: Intravenous fluconazole is typically administered once daily.
- Duration: The duration of treatment varies depending on the type of fungal infection being treated.
Duration of Treatment
The duration of treatment with fluconazole 200 mg depends on the type of fungal infection being treated. The following table provides a general overview of the typical duration of treatment for various fungal infections:
| Fungal Infection | Typical Duration of Treatment |
|---|---|
| Vaginal candidiasis | 1-3 days |
| Oral candidiasis (thrush) | 7-14 days |
| Cryptococcal meningitis | Several weeks or months |
| Coccidioidomycosis | Several months |
| Histoplasmosis | Several months |
| Blastomycosis | Several months |
Side Effects and Precautions of Fluconazole 200 mg

Fluconazole 200 mg, like any medication, can cause side effects and interactions. It is essential to be aware of these potential issues to ensure safe and effective treatment.
Common Side Effects
Common side effects of fluconazole 200 mg are usually mild and temporary.
- Headache
- Nausea
- Abdominal pain
- Diarrhea
- Rash
- Itching
Rare Side Effects
Rare side effects are less common but can be more serious.
- Liver problems, such as hepatitis
- Kidney problems
- Blood disorders
- Seizures
- Allergic reactions, including anaphylaxis
Drug Interactions
Fluconazole can interact with other medications, potentially affecting their effectiveness or increasing the risk of side effects.
- Warfarin: Fluconazole can increase the effects of warfarin, a blood thinner, leading to an increased risk of bleeding.
- Oral contraceptives: Fluconazole can decrease the effectiveness of oral contraceptives, potentially leading to unplanned pregnancy.
- Certain anti-rejection medications: Fluconazole can increase the levels of certain anti-rejection medications, potentially leading to side effects.
- Certain anti-seizure medications: Fluconazole can decrease the effectiveness of certain anti-seizure medications, potentially leading to seizures.
Precautions
Before starting fluconazole 200 mg treatment, it is crucial to inform your doctor about your medical history, including:
- Liver problems: Fluconazole can be harmful to the liver, and individuals with existing liver problems should use it with caution.
- Kidney problems: Fluconazole is excreted by the kidneys, and individuals with kidney problems may require dosage adjustments.
- Pregnancy: Fluconazole can harm a developing fetus, and it is generally not recommended during pregnancy.
- Breastfeeding: Fluconazole passes into breast milk, and it is not recommended for breastfeeding mothers.
- Allergies: Individuals with allergies to fluconazole or other azole antifungals should avoid using this medication.
Fluconazole 200 mg and Pregnancy
Fluconazole is an antifungal medication that is used to treat a variety of fungal infections. However, it is important to be aware of the potential risks of using fluconazole during pregnancy.
Potential Risks of Fluconazole During Pregnancy, Fluconazole 200 mg
Fluconazole can cross the placenta and reach the developing fetus. In some cases, this can lead to birth defects. The most common birth defects associated with fluconazole use during pregnancy are:
- Craniofacial abnormalities
- Cardiac defects
- Skeletal abnormalities
The risk of birth defects is higher when fluconazole is used during the first trimester of pregnancy.
Use of Fluconazole During Breastfeeding
Fluconazole is also excreted in breast milk. This means that it can be passed from the mother to the infant. It is important to discuss the risks and benefits of using fluconazole during breastfeeding with your doctor.
Managing Fungal Infections in Pregnant Women
If you are pregnant and have a fungal infection, your doctor will discuss the best treatment options with you. In some cases, they may recommend a different antifungal medication that is safer for pregnant women.
It is important to weigh the risks and benefits of using fluconazole during pregnancy. If you are pregnant or breastfeeding, talk to your doctor about the potential risks and benefits of using fluconazole.
Fluconazole 200 mg and Liver Function
Fluconazole, like many other medications, can potentially affect liver function. While it’s generally well-tolerated, some individuals may experience liver-related side effects. It’s crucial to understand the potential impact of fluconazole on the liver and the steps taken to minimize risks.
Hepatotoxicity Associated with Fluconazole 200 mg
Hepatotoxicity refers to liver damage caused by medications or other substances. Fluconazole can, in rare cases, lead to liver injury. The risk of hepatotoxicity is generally low, but it’s essential to be aware of the potential for this side effect.
- Fluconazole can cause a range of liver problems, including mild elevations in liver enzymes to more severe conditions like hepatitis or liver failure.
- The risk of hepatotoxicity appears to increase with higher doses and longer durations of fluconazole treatment.
- Individuals with pre-existing liver disease or those taking other medications known to affect the liver are at a higher risk of developing fluconazole-induced hepatotoxicity.
Monitoring Liver Function During Fluconazole Treatment
To minimize the risk of liver problems, healthcare professionals often monitor liver function during fluconazole treatment. This typically involves regular blood tests to check liver enzyme levels.
- Before starting fluconazole treatment, a baseline liver function test is usually performed.
- Liver function tests are typically repeated periodically during treatment, especially in patients at higher risk of hepatotoxicity.
- If any abnormalities in liver function tests are detected, the healthcare provider may adjust the fluconazole dose, discontinue the medication, or recommend further evaluation.
Fluconazole 200 mg and Drug Interactions
Fluconazole 200 mg, like many medications, can interact with other drugs, potentially altering their effectiveness or increasing the risk of side effects. Understanding these interactions is crucial for safe and effective medication use.
Drug Interactions with Fluconazole 200 mg
Fluconazole 200 mg can interact with various medications, affecting their metabolism, efficacy, or safety. This section Artikels common drug interactions with fluconazole 200 mg, their potential consequences, and recommendations for management.
Common Medications that Interact with Fluconazole 200 mg
The following table lists common medications that can interact with fluconazole 200 mg:
| Medication Class | Specific Medications | Potential Consequences |
|---|---|---|
| Anticoagulants | Warfarin, Coumadin | Increased risk of bleeding |
| Anti-epileptic Drugs | Phenytoin, Carbamazepine | Decreased effectiveness of anti-epileptic drugs |
| Immunosuppressants | Tacrolimus, Cyclosporine | Increased risk of organ rejection |
| Statins | Simvastatin, Lovastatin | Increased risk of muscle damage (myopathy) |
| Oral Hypoglycemics | Glipizide, Glyburide | Increased risk of hypoglycemia |
| Certain Anti-cancer Drugs | Vincristine, Vinblastine | Increased risk of neurotoxicity |
Consequences of Drug Interactions
The potential consequences of drug interactions with fluconazole 200 mg vary depending on the specific medications involved. Some common consequences include:
* Increased risk of side effects: This could involve an increased risk of bleeding, muscle damage, or other adverse reactions.
* Decreased effectiveness of medications: The interaction could reduce the effectiveness of other medications, such as anti-epileptic drugs or immunosuppressants.
* Increased risk of toxicity: Some interactions could lead to increased toxicity of other medications, such as anti-cancer drugs.
Managing Drug Interactions
To manage drug interactions with fluconazole 200 mg, it is crucial to:
* Inform your doctor about all medications you are taking: This includes prescription drugs, over-the-counter medications, herbal supplements, and vitamins.
* Monitor for side effects: Pay close attention to any new or worsening symptoms after starting fluconazole 200 mg.
* Adjust dosage or switch medications: Your doctor may need to adjust the dosage of fluconazole 200 mg or other medications or even switch to alternative medications to minimize the risk of interactions.
* Avoid grapefruit juice: Grapefruit juice can interact with fluconazole 200 mg and other medications, so it is best to avoid it while taking fluconazole 200 mg.
Fluconazole 200 mg and Resistance
The emergence of fungal resistance to fluconazole is a growing concern, particularly in patients with prolonged or recurrent infections. This resistance can significantly impact treatment outcomes and lead to more severe infections.
Mechanisms of Resistance Development
Fungal resistance to fluconazole can develop through various mechanisms. One primary mechanism involves mutations in the gene encoding for the enzyme lanosterol 14-α-demethylase (CYP51A1), which is the target of fluconazole. These mutations can reduce the affinity of fluconazole for the enzyme, leading to decreased inhibition of fungal growth. Another mechanism involves increased expression of efflux pumps, which actively transport fluconazole out of fungal cells, reducing its intracellular concentration.
Strategies for Managing Resistant Fungal Infections
Managing resistant fungal infections requires a multi-pronged approach:
- Susceptibility Testing: It is crucial to perform susceptibility testing to determine the antifungal susceptibility of the infecting organism. This helps guide the selection of appropriate antifungal agents.
- Combination Therapy: Combining fluconazole with other antifungal agents that target different pathways can be effective in overcoming resistance. For example, combining fluconazole with an echinocandin, such as caspofungin, can be beneficial.
- Alternative Antifungal Agents: If fluconazole resistance is confirmed, alternative antifungal agents, such as voriconazole, posaconazole, or itraconazole, may be considered. These agents have different mechanisms of action and may be effective against fluconazole-resistant strains.
- Prolonged Treatment Duration: In some cases, prolonged treatment duration may be necessary to achieve optimal therapeutic outcomes, particularly in patients with compromised immune systems.
- Infection Control Measures: Implementing strict infection control measures, such as hand hygiene and isolation precautions, can help prevent the spread of resistant strains.
Fluconazole 200 mg
Fluconazole 200 mg is a widely used antifungal medication, but it’s not the only option available. Understanding alternative treatments and the ongoing research in antifungal therapy is crucial for optimizing patient care.
Alternatives to Fluconazole 200 mg
Various antifungal medications exist, each with its own strengths and limitations. Choosing the best option depends on the specific fungal infection, patient factors, and potential drug interactions.
- Itraconazole: Available in oral and intravenous forms, itraconazole is effective against a broad spectrum of fungal infections, including those caused by *Aspergillus* and *Candida* species. Itraconazole is often used for treating onychomycosis (nail fungus) and is also effective against *Blastomyces dermatitidis* and *Histoplasma capsulatum* infections.
- Voriconazole: Primarily administered intravenously, voriconazole is particularly effective against invasive aspergillosis, a serious fungal infection that can affect the lungs and other organs. It’s also used for treating candidemia (Candida infection in the bloodstream) and other *Candida* infections.
- Posaconazole: Available in oral and intravenous forms, posaconazole is broad-spectrum and is commonly used for prophylaxis (prevention) of invasive fungal infections in high-risk patients, such as those undergoing bone marrow transplantation or those with weakened immune systems.
- Caspofungin: This echinocandin antifungal is administered intravenously and is primarily used for treating invasive candidiasis and aspergillosis. It’s also effective against *Candida* infections that are resistant to other antifungals.
- Micafungin: Another echinocandin antifungal, micafungin is administered intravenously and is used for similar indications as caspofungin, including invasive candidiasis and aspergillosis.
Comparison of Antifungal Agents
Comparing antifungal medications involves considering their effectiveness, side effects, and administration routes.
| Antifungal Agent | Effectiveness | Side Effects | Administration |
|---|---|---|---|
| Fluconazole | Effective against various *Candida* infections, including oral thrush, vaginal yeast infections, and cryptococcal meningitis. | Nausea, vomiting, diarrhea, headache, rash, and liver problems. | Oral, intravenous |
| Itraconazole | Broad-spectrum antifungal, effective against *Aspergillus*, *Candida*, *Blastomyces*, and *Histoplasma* infections. | Nausea, vomiting, diarrhea, headache, rash, and liver problems. | Oral, intravenous |
| Voriconazole | Effective against invasive aspergillosis, candidemia, and other *Candida* infections. | Visual disturbances, hallucinations, rash, and liver problems. | Intravenous |
| Posaconazole | Broad-spectrum antifungal, effective against *Aspergillus*, *Candida*, and *Mucorales* infections. | Nausea, vomiting, diarrhea, headache, and liver problems. | Oral, intravenous |
| Caspofungin | Effective against invasive candidiasis and aspergillosis. | Nausea, vomiting, headache, and liver problems. | Intravenous |
| Micafungin | Effective against invasive candidiasis and aspergillosis. | Nausea, vomiting, headache, and liver problems. | Intravenous |
Future Directions in Antifungal Therapy
Research continues to explore new antifungal therapies and strategies to address the challenges posed by emerging fungal infections and drug resistance.
- Novel Antifungal Targets: Scientists are investigating new targets within fungal cells that could be exploited for drug development. This includes exploring the unique metabolic pathways and cellular processes of fungi to identify specific vulnerabilities that can be targeted with novel antifungal agents.
- Combination Therapies: Combining different antifungal agents with distinct mechanisms of action can potentially enhance efficacy and overcome drug resistance. This approach aims to target multiple pathways within fungal cells, making it more difficult for the fungus to develop resistance.
- Personalized Antifungal Therapy: The development of personalized antifungal therapy is driven by the need to tailor treatment based on individual patient characteristics and the specific fungal infection. This could involve using genetic testing to identify fungal species and predict drug resistance, allowing for more targeted and effective treatment.
- Nanotechnology in Antifungal Delivery: Nanotechnology offers innovative approaches for delivering antifungal agents directly to the site of infection, potentially increasing efficacy and reducing side effects. This could involve using nanoparticles to encapsulate antifungal drugs, enhancing their penetration into fungal cells and minimizing their impact on healthy tissues.
Fluconazole 200 mg has proven to be a valuable asset in the fight against fungal infections, offering effective treatment for a variety of conditions. While generally safe and well-tolerated, it’s essential to be aware of potential side effects, drug interactions, and the importance of monitoring liver function during treatment. Ongoing research continues to explore new avenues for antifungal therapies, aiming to enhance treatment effectiveness and minimize adverse effects. By understanding the intricacies of fluconazole 200 mg, healthcare professionals and patients can work together to optimize treatment outcomes and ensure the well-being of individuals facing fungal infections.
Fluconazole 200 mg is a common antifungal medication used to treat a variety of fungal infections. While fluconazole targets fungal cells, evolocumab focuses on reducing cholesterol levels by targeting a specific protein in the body. Both medications are important in their respective fields, highlighting the diversity of treatments available for different health conditions.