Bisphosphonates are a class of drugs that work to prevent bone loss and strengthen bones. These medications are primarily used to treat osteoporosis, a condition that weakens bones and increases the risk of fractures. Bisphosphonates work by slowing down the breakdown of bone tissue, which helps to increase bone density and reduce the risk of fractures.
Bisphosphonates are available in various forms, including oral pills, intravenous infusions, and injections. The choice of medication and delivery method depends on the individual’s condition and needs. They have proven to be effective in treating a range of bone conditions, but it’s important to understand their potential side effects and interactions with other medications.
What are Bisphosphonates?
Bisphosphonates are a class of drugs that are used to treat osteoporosis, Paget’s disease of bone, and certain types of cancer that have spread to the bones. They work by inhibiting the activity of osteoclasts, the cells responsible for breaking down bone. This slows down bone loss and can help to increase bone density.
Chemical Structure and Mechanism of Action
Bisphosphonates are structurally similar to pyrophosphate, a natural inhibitor of bone resorption. They contain a carbon-phosphorus-phosphorus bond (C-P-P) that is crucial for their activity. This bond allows bisphosphonates to bind to hydroxyapatite, the mineral component of bone, and inhibit the activity of osteoclasts.
Bisphosphonates are analogs of pyrophosphate, a natural inhibitor of bone resorption. They contain a carbon-phosphorus-phosphorus bond (C-P-P) that is crucial for their activity. This bond allows bisphosphonates to bind to hydroxyapatite, the mineral component of bone, and inhibit the activity of osteoclasts.
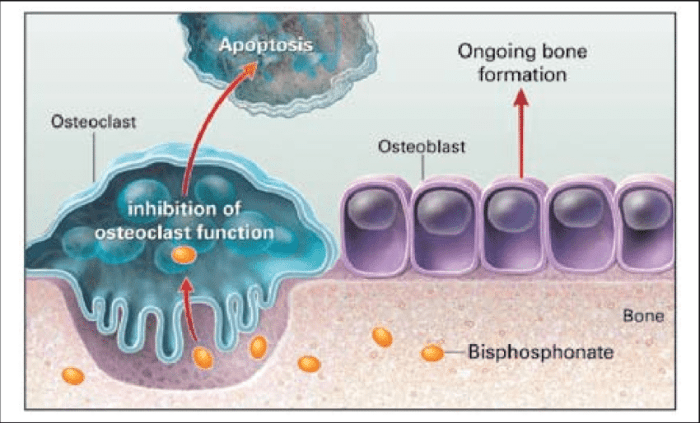
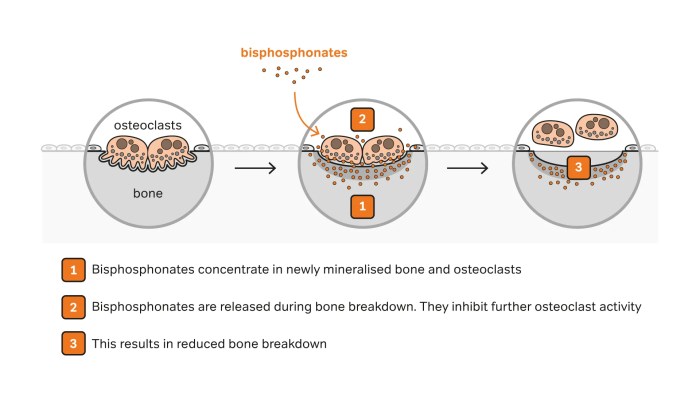
The mechanism of action of bisphosphonates involves several steps:
1. Binding to hydroxyapatite: Bisphosphonates bind to hydroxyapatite crystals in bone, which are the main component of the bone matrix.
2. Inhibition of osteoclast activity: Once bound to bone, bisphosphonates are taken up by osteoclasts, the cells responsible for bone resorption. This uptake leads to the inhibition of osteoclast activity, preventing bone breakdown.
3. Increased bone density: The inhibition of bone resorption leads to a decrease in bone turnover and an increase in bone density.
Types of Bisphosphonates and Their Uses
There are many different types of bisphosphonates, each with its own specific uses. Here are some examples:
- Alendronate (Fosamax): Alendronate is a widely used bisphosphonate for the treatment of osteoporosis in both men and women. It is also used to treat Paget’s disease of bone.
- Risedronate (Actonel): Risedronate is another common bisphosphonate used for the treatment of osteoporosis. It is also available in a once-monthly dosage form.
- Ibandronate (Boniva): Ibandronate is a bisphosphonate that is available in both oral and intravenous formulations. It is used to treat osteoporosis and to prevent bone loss in women who are at high risk for developing the condition.
- Zoledronic acid (Reclast): Zoledronic acid is a potent bisphosphonate that is administered intravenously. It is used to treat osteoporosis, Paget’s disease of bone, and certain types of cancer that have spread to the bones.
- Pamidronate (Aredia): Pamidronate is a bisphosphonate that is used to treat Paget’s disease of bone and to prevent bone loss in patients with multiple myeloma.
Bisphosphonates are effective medications for treating osteoporosis and other bone diseases. They work by inhibiting the activity of osteoclasts, the cells responsible for breaking down bone. This slows down bone loss and can help to increase bone density.
Clinical Applications of Bisphosphonates
Bisphosphonates are a class of drugs that are used to treat a variety of bone diseases. They work by inhibiting the activity of osteoclasts, the cells responsible for breaking down bone. This action helps to slow down bone loss and promote bone formation.
Treatment of Osteoporosis
Bisphosphonates are a mainstay in the treatment of osteoporosis, a condition characterized by low bone density and an increased risk of fractures. They are effective in reducing the risk of fractures, particularly in the spine, hip, and wrist.
Bisphosphonates are typically prescribed for long-term use, often for several years, to maintain bone density and reduce fracture risk.
- Alendronate (Fosamax): Alendronate is a widely used bisphosphonate for the treatment of osteoporosis. It is available in oral and intravenous formulations.
- Risedronate (Actonel): Risedronate is another commonly prescribed bisphosphonate. It is available in oral and intravenous formulations.
- Ibandronate (Boniva): Ibandronate is a bisphosphonate that can be taken orally or intravenously. It is often used to treat osteoporosis in postmenopausal women.
- Zoledronic acid (Reclast): Zoledronic acid is a potent bisphosphonate that is administered intravenously. It is typically given once a year for the treatment of osteoporosis.
Management of Paget’s Disease of Bone
Paget’s disease of bone is a chronic condition that causes excessive bone turnover. Bisphosphonates are effective in treating Paget’s disease by slowing down the rate of bone breakdown and promoting bone formation.
Bisphosphonates can help to reduce pain, prevent bone deformities, and decrease the risk of fractures in patients with Paget’s disease.
- Tiludronate (Skelid): Tiludronate is a bisphosphonate that is specifically approved for the treatment of Paget’s disease.
- Pamidronate (Aredia): Pamidronate is another bisphosphonate that is used to treat Paget’s disease. It is administered intravenously.
- Zoledronic acid (Reclast): Zoledronic acid is also effective in treating Paget’s disease. It is given intravenously, typically as a single infusion.
Prevention and Treatment of Bone Metastases
Bone metastases are cancer cells that have spread from a primary tumor to the bones. Bisphosphonates are used to prevent and treat bone metastases, particularly in cancers such as breast cancer, prostate cancer, and lung cancer.
Bisphosphonates can help to reduce pain, prevent fractures, and improve quality of life in patients with bone metastases.
- Zoledronic acid (Reclast): Zoledronic acid is a commonly used bisphosphonate for the prevention and treatment of bone metastases.
- Pamidronate (Aredia): Pamidronate is another bisphosphonate that is used to treat bone metastases.
Pharmacokinetics and Administration
Bisphosphonates are a class of drugs that are used to treat a variety of bone diseases. They work by inhibiting the activity of osteoclasts, the cells that break down bone. This slows down bone resorption and helps to maintain bone density. Understanding the pharmacokinetics of bisphosphonates is crucial for optimizing their therapeutic efficacy and minimizing potential adverse effects.
Absorption
Bisphosphonates are poorly absorbed from the gastrointestinal tract. Their absorption is highly dependent on factors such as the chemical structure of the specific bisphosphonate, the presence of food, and the pH of the stomach. The oral bioavailability of bisphosphonates is typically low, ranging from 1% to 15%.
- The presence of food, especially calcium-rich foods, significantly reduces the absorption of bisphosphonates. This is because calcium binds to the bisphosphonates in the gastrointestinal tract, forming insoluble complexes that cannot be absorbed.
- The pH of the stomach also plays a role in the absorption of bisphosphonates. Bisphosphonates are more soluble in acidic environments, so they are better absorbed in the stomach than in the intestines.
Distribution
After absorption, bisphosphonates are widely distributed throughout the body, with a high affinity for bone. They accumulate in bone tissue, where they exert their therapeutic effects. Bisphosphonates have a long half-life in bone, ranging from months to years.
- Once bisphosphonates bind to bone, they are slowly released back into the circulation.
- The long half-life of bisphosphonates in bone explains their prolonged therapeutic effect and allows for infrequent dosing regimens.
Metabolism
Bisphosphonates are not significantly metabolized in the body. They are primarily excreted unchanged in the urine.
- The kidneys are the primary route of excretion for bisphosphonates.
- Renal impairment can lead to an accumulation of bisphosphonates in the body, increasing the risk of adverse effects.
Excretion
Bisphosphonates are primarily excreted unchanged in the urine. The rate of excretion is dependent on renal function.
- Patients with impaired renal function may experience a slower rate of bisphosphonate excretion, leading to higher drug levels in the body and an increased risk of adverse effects.
- The half-life of bisphosphonates can be significantly prolonged in patients with renal impairment.
Routes of Administration
Bisphosphonates are available in both oral and intravenous formulations. The choice of route of administration depends on the specific bisphosphonate, the patient’s condition, and the desired therapeutic effect.
- Oral bisphosphonates are typically used for the treatment of osteoporosis and Paget’s disease of bone.
- Intravenous bisphosphonates are often used for the treatment of more severe bone diseases, such as metastatic bone disease and multiple myeloma.
Factors Affecting Bioavailability and Efficacy
Several factors can affect the bioavailability and efficacy of bisphosphonates. These include:
- The chemical structure of the specific bisphosphonate
- The presence of food in the gastrointestinal tract
- The pH of the stomach
- Renal function
- Patient compliance with medication regimen
Adverse Effects and Precautions
Bisphosphonates, while generally safe and effective, can cause a range of adverse effects, some of which can be serious. Understanding these potential risks and implementing appropriate precautions is crucial for ensuring patient safety and optimizing treatment outcomes.
Common Adverse Effects
Common adverse effects associated with bisphosphonate use are generally mild and often resolve with continued treatment.
- Gastrointestinal Disturbances: Bisphosphonates can irritate the gastrointestinal tract, leading to nausea, vomiting, dyspepsia, and esophagitis. These effects are more common with oral bisphosphonates, particularly if taken without adequate water intake or on an empty stomach.
- Musculoskeletal Pain: Some patients may experience musculoskeletal pain, particularly in the bones, muscles, and joints. This pain can be localized or widespread and may be exacerbated by exercise or activity.
- Hypocalcemia: Bisphosphonates can interfere with calcium absorption, potentially leading to hypocalcemia. This is more likely to occur in patients with underlying calcium deficiency or those receiving high doses of bisphosphonates.
Serious Adverse Effects
While less common, serious adverse effects can occur with bisphosphonate use. These effects require prompt medical attention.
- Osteonecrosis of the Jaw (ONJ): This is a rare but serious complication characterized by bone death in the jaw. ONJ is more likely to occur in patients with compromised oral health, those receiving high doses of bisphosphonates, and those undergoing dental procedures.
- Atypical Femoral Fractures: Bisphosphonates can increase the risk of atypical femoral fractures, which are stress fractures that occur in the subtrochanteric or diaphyseal regions of the femur. These fractures often occur without significant trauma and may be associated with pain and tenderness in the thigh.
- Esophageal Ulceration: Oral bisphosphonates can cause esophageal ulceration, particularly if they are not taken with adequate water intake or on an empty stomach. This complication can lead to severe pain, difficulty swallowing, and bleeding.
- Hypophosphatemia: Bisphosphonates can interfere with phosphate absorption, leading to hypophosphatemia. This is more likely to occur in patients with underlying phosphate deficiency or those receiving high doses of bisphosphonates.
Drug Interactions
Bisphosphonates can interact with other medications, potentially increasing the risk of adverse effects. It is essential to inform healthcare providers of all medications, including over-the-counter drugs, supplements, and herbal remedies, being taken before starting bisphosphonate therapy.
- Calcium Supplements: Bisphosphonates can reduce calcium absorption, so concurrent use of calcium supplements may be necessary to maintain adequate calcium levels.
- Antacids: Antacids containing aluminum, magnesium, or calcium can interfere with the absorption of oral bisphosphonates. It is recommended to take bisphosphonates at least 30 minutes before or 2 hours after antacids.
- Other Medications: Bisphosphonates can interact with other medications, such as certain antibiotics, diuretics, and corticosteroids.
Monitoring and Management
Patients on bisphosphonate therapy require careful monitoring to identify and manage potential adverse effects.
- Baseline Assessments: Before starting bisphosphonate therapy, it is essential to assess the patient’s overall health, including dental health, bone density, and calcium and phosphate levels.
- Regular Monitoring: Patients should undergo regular monitoring during bisphosphonate therapy, including dental checkups, bone density assessments, and blood tests to assess calcium and phosphate levels.
- Early Intervention: If any adverse effects are detected, prompt medical attention is essential to manage the condition and prevent further complications.
Bisphosphonates and Bone Health
Bisphosphonates are a class of drugs that have revolutionized the treatment of osteoporosis and other bone disorders. Their primary mechanism of action involves inhibiting bone resorption, the process by which old bone tissue is broken down. This leads to an increase in bone density and a reduction in fracture risk.
Impact on Bone Density and Fracture Risk
Bisphosphonates have been shown to significantly increase bone mineral density (BMD) in patients with osteoporosis. Studies have demonstrated that bisphosphonates can increase BMD by 5-10% in the spine and hip, which are the areas most susceptible to fractures. This increase in BMD is associated with a reduction in fracture risk, particularly in the spine, hip, and wrist. For instance, a large meta-analysis of clinical trials found that bisphosphonates reduced the risk of vertebral fractures by 50% and hip fractures by 30-40%.
Long-Term Effects of Bisphosphonate Therapy on Bone Health
The long-term effects of bisphosphonate therapy on bone health are complex and still being investigated. While bisphosphonates are effective in increasing BMD and reducing fracture risk in the short term, there is some evidence suggesting that long-term use may be associated with an increased risk of atypical femoral fractures. These are fractures that occur in the femoral shaft, often in patients who have been on bisphosphonates for several years. However, the incidence of atypical femoral fractures is still relatively low, and the benefits of bisphosphonate therapy in reducing osteoporosis-related fractures generally outweigh the risks.
Efficacy of Different Bisphosphonates in Improving Bone Mineral Density
Different bisphosphonates have varying efficacies in improving BMD. Some of the commonly used bisphosphonates include alendronate, risedronate, zoledronic acid, and ibandronate. Alendronate and risedronate are oral bisphosphonates, while zoledronic acid and ibandronate are intravenous bisphosphonates. The choice of bisphosphonate depends on the individual patient’s needs and preferences.
The efficacy of bisphosphonates in improving BMD is influenced by factors such as the dose, route of administration, and duration of treatment.
- Alendronate and risedronate are generally effective in increasing BMD in the spine and hip, but their effects on other skeletal sites may be less pronounced.
- Zoledronic acid and ibandronate are more potent bisphosphonates and can lead to greater increases in BMD, particularly in the spine.
It’s important to note that the choice of bisphosphonate should be made in consultation with a healthcare professional, taking into account individual factors such as the patient’s risk of fracture, medical history, and potential side effects.
Bisphosphonates have revolutionized the treatment of osteoporosis and other bone disorders, providing patients with a valuable tool for maintaining bone health and reducing fracture risk. However, it’s crucial to use these medications under the guidance of a healthcare professional, considering individual factors and potential side effects. Understanding the benefits and risks of bisphosphonates is key to making informed decisions about bone health management.
Bisphosphonates are a class of drugs used to treat osteoporosis, a condition that weakens bones. While they work on bone health, it’s important to remember that they don’t address respiratory conditions like asthma, which is often treated with medications like montelukast. Bisphosphonates are generally well-tolerated, but like any medication, they can have side effects. It’s crucial to discuss your individual needs and risks with your doctor before starting any new treatment.