Mycophenolate, a powerful immunosuppressant, has revolutionized the treatment of organ transplantation and autoimmune diseases. This drug works by inhibiting the production of purines, essential building blocks for DNA and RNA, thereby suppressing the immune system’s ability to attack foreign cells or tissues.
Mycophenolate is available in various formulations, including oral tablets and intravenous preparations, allowing for tailored treatment regimens based on individual patient needs. Its efficacy has been well-established in numerous clinical settings, and ongoing research continues to explore its potential in new therapeutic areas.
Mycophenolate
Mycophenolate is an immunosuppressant medication commonly used to prevent organ rejection after transplantation and to treat autoimmune diseases. It functions by inhibiting the synthesis of purines, essential building blocks for DNA and RNA, thus disrupting the proliferation of immune cells.
Chemical Structure and Properties
Mycophenolate is a derivative of mycophenolic acid, a natural product produced by the fungus *Penicillium brevicompactum*. Its chemical structure consists of a phenyl ring attached to a substituted cyclohexane ring. Mycophenolate is a white, crystalline powder that is practically insoluble in water but soluble in organic solvents such as methanol and ethanol.
Mechanism of Action, Mycophenolate
Mycophenolate exerts its immunosuppressive effects by inhibiting the enzyme inosine monophosphate dehydrogenase (IMPDH), which is crucial for the synthesis of guanine nucleotides. Specifically, mycophenolate targets the active site of IMPDH, preventing the conversion of inosine monophosphate (IMP) to guanosine monophosphate (GMP).
GMP is a vital precursor for DNA and RNA synthesis, and its depletion leads to a reduction in the proliferation of immune cells, particularly T lymphocytes and B lymphocytes.
Formulations of Mycophenolate
Mycophenolate is available in two main formulations:
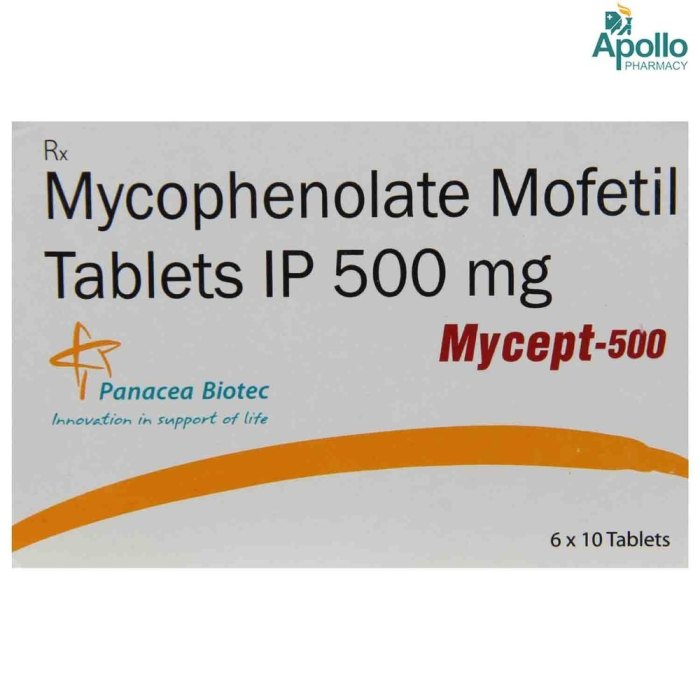
- Mycophenolate mofetil (MMF): MMF is the prodrug form of mycophenolate. It is readily absorbed orally and converted to mycophenolic acid in the body. MMF is typically administered twice daily.
- Mycophenolic acid (MPA): MPA is the active form of mycophenolate. It is available as an oral suspension and an intravenous formulation. MPA is typically administered once daily.
Therapeutic Applications of Mycophenolate
Mycophenolate is an immunosuppressant medication that works by inhibiting the production of purine nucleotides, essential molecules involved in cell growth and proliferation. This mechanism of action makes mycophenolate a powerful tool for suppressing the immune system, making it a valuable treatment option for a range of conditions.
Organ Transplantation
Mycophenolate is a cornerstone of immunosuppressive therapy for organ transplantation. It is typically used in combination with other immunosuppressants, such as cyclosporine or tacrolimus, to prevent rejection of the transplanted organ. Mycophenolate’s effectiveness in preventing rejection has been well-established in numerous clinical trials, and it has become a standard of care in the management of organ transplant recipients.
Autoimmune Diseases
Mycophenolate has also proven effective in the treatment of various autoimmune diseases. Its ability to suppress the immune system makes it a suitable option for conditions where the body’s immune system attacks its own tissues. Mycophenolate has been used to treat a wide range of autoimmune diseases, including:
- Systemic lupus erythematosus (SLE): Mycophenolate is an effective treatment for lupus nephritis, a serious complication of SLE that affects the kidneys. It helps to reduce inflammation and prevent further damage to the kidneys.
- Rheumatoid arthritis (RA): Mycophenolate is used in combination with other medications, such as methotrexate, to treat RA. It helps to reduce joint pain, swelling, and stiffness.
- Crohn’s disease and ulcerative colitis: Mycophenolate is an effective treatment for moderate to severe Crohn’s disease and ulcerative colitis, particularly in cases that are unresponsive to conventional therapies.
- Vasculitis: Mycophenolate can be used to treat certain types of vasculitis, a group of diseases that cause inflammation of the blood vessels.
- Myasthenia gravis: Mycophenolate has been used in some cases to treat myasthenia gravis, an autoimmune disorder that affects the muscles.
Off-Label Uses
Mycophenolate has also been used off-label for a variety of other conditions, including:
- Psoriasis: Some studies have suggested that mycophenolate may be effective in treating severe psoriasis, a chronic skin condition characterized by scaly patches.
- Scleroderma: Mycophenolate has been used in some cases to treat scleroderma, a rare autoimmune disease that causes hardening of the skin and other tissues.
- Multiple sclerosis: Mycophenolate has been investigated as a potential treatment for multiple sclerosis, an autoimmune disease that affects the central nervous system.
Pharmacokinetic and Pharmacodynamic Properties
Mycophenolate, a potent immunosuppressant, exhibits a unique pharmacokinetic profile and exerts its therapeutic effects by modulating the immune system. Understanding its pharmacokinetic and pharmacodynamic properties is crucial for optimizing its therapeutic use and minimizing potential adverse effects.
Pharmacokinetic Profile
Mycophenolate’s pharmacokinetic profile describes its movement within the body, encompassing absorption, distribution, metabolism, and excretion.
- Absorption: Mycophenolate mofetil (MMF), the prodrug form, is well-absorbed after oral administration, reaching peak plasma concentrations within 1-2 hours. However, its bioavailability is highly variable, ranging from 20% to 90%, primarily due to first-pass metabolism in the gut and liver. Food can significantly impact absorption, leading to a decrease in peak concentrations and a slower absorption rate. Therefore, MMF should be administered on an empty stomach.
- Distribution: Mycophenolate’s active metabolite, mycophenolic acid (MPA), distributes widely into various tissues, including the kidneys, liver, lungs, and spleen. It exhibits a relatively low volume of distribution, suggesting that it is primarily confined to the plasma and interstitial fluids.
- Metabolism: MPA undergoes extensive metabolism primarily by glucuronidation, resulting in the formation of inactive metabolites. This metabolic pathway is responsible for the short half-life of MPA, which is approximately 12-16 hours. However, MPA can also be metabolized by other pathways, including oxidation and hydrolysis, which can contribute to interindividual variability in drug clearance.
- Excretion: MPA and its metabolites are primarily excreted in the urine, with a small amount excreted in the feces. Renal function significantly influences MPA elimination, with decreased renal function leading to increased drug accumulation and potential toxicity. Therefore, close monitoring of renal function is essential during mycophenolate therapy.
Pharmacodynamic Effects
Mycophenolate exerts its immunosuppressive effects by inhibiting inosine monophosphate dehydrogenase (IMPDH), a key enzyme involved in the de novo synthesis of guanine nucleotides. This inhibition disrupts the production of DNA and RNA, leading to impaired proliferation of lymphocytes, particularly T cells.
- T-cell suppression: Mycophenolate preferentially inhibits the proliferation of activated T cells, which are crucial for the initiation and amplification of immune responses. By reducing T-cell activation and proliferation, mycophenolate effectively suppresses both humoral and cellular immunity.
- B-cell suppression: While mycophenolate primarily targets T cells, it also exhibits some inhibitory effects on B-cell function. It can suppress antibody production and reduce the formation of memory B cells, further contributing to its immunosuppressive effects.
Drug Interactions
Mycophenolate’s metabolism and excretion can be influenced by various drugs, potentially impacting its efficacy and increasing the risk of adverse effects.
- Drugs that inhibit glucuronidation: Concomitant use of drugs that inhibit glucuronidation, such as cimetidine, probenecid, and some antibiotics, can increase MPA levels, potentially leading to toxicity. Therefore, careful monitoring of MPA levels and dose adjustments may be necessary.
- Drugs that induce glucuronidation: Drugs that induce glucuronidation, such as rifampicin and phenytoin, can reduce MPA levels, potentially compromising its therapeutic efficacy. Monitoring MPA levels and dose adjustments may be required to maintain therapeutic efficacy.
- Drugs that affect renal function: Drugs that affect renal function, such as aminoglycosides and NSAIDs, can increase MPA accumulation and the risk of toxicity. Close monitoring of renal function and potential dose adjustments are crucial when mycophenolate is used in conjunction with these drugs.
Adverse Effects and Safety Considerations

Mycophenolate, while effective in preventing transplant rejection, can cause a range of adverse effects, some of which can be serious. Understanding these potential risks and implementing appropriate monitoring strategies are crucial for minimizing complications and optimizing patient outcomes.
Common Adverse Effects
Common adverse effects of mycophenolate therapy are generally mild and manageable. They are frequently encountered and usually resolve with adjustments to the dosage or supportive care.
- Gastrointestinal Disturbances: Nausea, vomiting, diarrhea, and abdominal pain are among the most prevalent side effects. These symptoms are often dose-dependent and may improve with lower doses or the use of antiemetics.
- Hematologic Effects: Mycophenolate can suppress bone marrow function, leading to leukopenia (low white blood cell count), anemia (low red blood cell count), and thrombocytopenia (low platelet count). Regular blood monitoring is essential to detect and manage these potential complications.
- Infections: Mycophenolate’s immunosuppressive properties increase the risk of infections. Patients should be closely monitored for signs of infection, and prompt treatment is crucial.
Serious Adverse Effects
While less common, serious adverse effects of mycophenolate can have significant implications for patient health. Early recognition and prompt management are vital to minimize the severity of these complications.
- Opportunistic Infections: Due to its immunosuppressive nature, mycophenolate increases the susceptibility to opportunistic infections, such as cytomegalovirus (CMV) and Pneumocystis jirovecii pneumonia (PCP). Prophylactic measures and close monitoring are essential to prevent these infections.
- Lymphoma: There is a potential increased risk of lymphoma, particularly in patients with long-term mycophenolate therapy. Regular monitoring for any signs of lymphoma is recommended.
- Hepatotoxicity: Mycophenolate can cause liver damage, although this is rare. Liver function tests should be monitored regularly to detect any abnormalities.
- Teratogenicity: Mycophenolate is highly teratogenic and can cause severe birth defects. It is contraindicated in women of childbearing potential unless adequate contraception is used.
Monitoring Parameters
Regular monitoring is essential to minimize the risks and optimize the benefits of mycophenolate therapy.
- Complete Blood Count (CBC): Regular CBC monitoring is crucial to assess for hematologic effects, such as leukopenia, anemia, and thrombocytopenia. Adjustments to the dosage or supportive care may be necessary based on the results.
- Liver Function Tests (LFTs): LFTs should be monitored regularly to detect any signs of liver damage, particularly in patients with pre-existing liver disease.
- Renal Function Tests: Mycophenolate can affect kidney function. Regular monitoring of creatinine and other renal function parameters is essential.
- Infections: Patients should be closely monitored for signs of infection, including fever, chills, cough, dyspnea, and pain. Prompt treatment is crucial to prevent complications.
Managing Potential Adverse Events
The management of adverse events associated with mycophenolate therapy depends on the severity and nature of the event.
- Gastrointestinal Disturbances: Mild gastrointestinal symptoms can often be managed with dietary modifications and antiemetics. In severe cases, a temporary dose reduction or discontinuation of mycophenolate may be necessary.
- Hematologic Effects: Hematologic effects are managed by monitoring CBCs and adjusting the dosage or providing supportive care, such as blood transfusions. In some cases, a temporary or permanent discontinuation of mycophenolate may be required.
- Infections: Prompt diagnosis and treatment of infections are crucial. This may involve antibiotic therapy, antiviral agents, or antifungal medications, depending on the type of infection.
- Opportunistic Infections: Prophylactic measures, such as antiviral medications or anti-Pneumocystis jirovecii prophylaxis, can help prevent opportunistic infections. Close monitoring for signs of infection is essential.
- Lymphoma: If lymphoma is suspected, prompt evaluation and treatment are crucial. The management of lymphoma depends on the type and stage of the disease.
- Hepatotoxicity: In cases of hepatotoxicity, mycophenolate may need to be discontinued or the dosage adjusted. Supportive care, such as liver transplantation, may be necessary in severe cases.
- Teratogenicity: Effective contraception is crucial for women of childbearing potential taking mycophenolate. Patients should be counseled about the risks of teratogenicity and the importance of reliable contraception.
Mycophenolate in the Context of Organ Transplantation
Mycophenolate is a cornerstone of immunosuppressive therapy in organ transplantation, playing a crucial role in preventing rejection of the transplanted organ. Its mechanism of action, targeting purine synthesis, effectively suppresses the immune response that would otherwise attack the foreign tissue. This section delves into the role of mycophenolate in transplantation, comparing it with other immunosuppressive agents and examining its long-term impact on graft survival and patient health.
Mycophenolate’s Role in Preventing Organ Rejection
Mycophenolate, specifically mycophenolate mofetil (MMF), is a potent immunosuppressant commonly used in conjunction with other medications, such as calcineurin inhibitors (e.g., cyclosporine or tacrolimus) and corticosteroids, to prevent organ rejection. It achieves this by selectively inhibiting the proliferation of T lymphocytes, a key component of the immune system responsible for recognizing and attacking foreign antigens. By blocking the production of purines, essential building blocks for DNA and RNA, mycophenolate effectively halts the rapid division of T cells, thereby suppressing the immune response against the transplanted organ.
Comparison with Other Immunosuppressive Agents
Mycophenolate, when compared to other immunosuppressants used in transplantation, offers several advantages. For instance, it has a relatively low incidence of nephrotoxicity, a concern with calcineurin inhibitors. Additionally, mycophenolate exhibits a more favorable safety profile regarding cardiovascular complications compared to other agents like azathioprine.
- Calcineurin inhibitors (cyclosporine, tacrolimus): While effective, these agents carry a higher risk of nephrotoxicity and hypertension.
- Azathioprine: Although generally well-tolerated, azathioprine has a higher risk of bone marrow suppression and can interact with certain medications.
- Corticosteroids: These agents are often used in combination with other immunosuppressants to manage inflammation and acute rejection episodes. However, long-term corticosteroid use can lead to metabolic side effects.
Long-Term Impact on Graft Survival and Patient Health
Mycophenolate has demonstrated significant contributions to improving graft survival and patient health in the long term. Numerous studies have shown that mycophenolate-based regimens have led to improved graft function and reduced rejection rates compared to older immunosuppressive regimens. This has translated into better long-term outcomes for transplant recipients, including improved quality of life and increased survival rates. However, long-term mycophenolate use can be associated with potential adverse effects, including gastrointestinal disturbances, bone marrow suppression, and an increased risk of infections. Therefore, careful monitoring and management are essential to minimize these risks and optimize patient outcomes.
Mycophenolate in Autoimmune Diseases
Mycophenolate mofetil (MMF) is an immunosuppressant medication that has emerged as a valuable therapeutic option in the management of autoimmune diseases. Its mechanism of action, targeting the purine synthesis pathway, makes it effective in suppressing the immune system’s aberrant responses that contribute to the pathogenesis of various autoimmune conditions.
Rationale for Using Mycophenolate in Autoimmune Diseases
Mycophenolate’s effectiveness in autoimmune diseases stems from its ability to selectively inhibit the proliferation of lymphocytes, specifically T and B cells, which play a central role in the development and progression of autoimmune disorders. By interfering with the production of purines, essential building blocks for DNA synthesis, mycophenolate effectively prevents the clonal expansion of activated lymphocytes, thereby reducing the overall immune response.
Specific Autoimmune Conditions Where Mycophenolate is Indicated
Mycophenolate has demonstrated clinical efficacy in the treatment of a range of autoimmune diseases, including:
- Systemic Lupus Erythematosus (SLE): Mycophenolate is often used in combination with other immunosuppressants to manage SLE, particularly in cases with severe disease activity or resistance to conventional therapies. It helps control the inflammatory process and reduce the frequency and severity of lupus flares.
- Rheumatoid Arthritis (RA): Mycophenolate is a valuable alternative for patients with RA who do not respond adequately to traditional disease-modifying antirheumatic drugs (DMARDs). It effectively reduces joint inflammation, pain, and stiffness, improving overall functional capacity.
- Crohn’s Disease and Ulcerative Colitis (Inflammatory Bowel Diseases, IBD): Mycophenolate is frequently used in patients with IBD, especially those with moderate to severe disease activity. It helps to suppress the inflammatory process in the gastrointestinal tract, reducing symptoms like abdominal pain, diarrhea, and rectal bleeding.
- Vasculitis: Mycophenolate has shown promise in the treatment of certain types of vasculitis, including granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA). It helps to control inflammation and prevent further tissue damage caused by the disease.
- Myasthenia Gravis: Mycophenolate is sometimes used as an adjunct therapy in patients with myasthenia gravis, a neuromuscular disorder characterized by muscle weakness. It can help reduce the severity of symptoms and improve muscle strength.
Effectiveness of Mycophenolate in Managing Autoimmune Disease Symptoms
Clinical studies have consistently demonstrated the effectiveness of mycophenolate in managing autoimmune disease symptoms. For example, in patients with SLE, mycophenolate has been shown to reduce disease activity, improve quality of life, and decrease the need for corticosteroids. In RA, mycophenolate has been associated with significant improvements in joint pain, swelling, and physical function. Similarly, in IBD, mycophenolate has been shown to induce remission, reduce the frequency of flares, and improve patient-reported outcomes.
It’s important to note that mycophenolate is generally not a first-line treatment for autoimmune diseases. It is typically used when other therapies have failed or are not suitable for the patient.
Future Directions in Mycophenolate Research
Mycophenolate mofetil (MMF) has emerged as a cornerstone immunosuppressant in organ transplantation and the management of autoimmune diseases. Its efficacy and safety profile have led to its widespread adoption, but ongoing research continues to explore avenues for optimizing its therapeutic potential. These efforts aim to enhance its formulation, delivery, and efficacy, and to develop novel therapeutic strategies involving MMF.
Formulations and Delivery Systems
The development of novel formulations and delivery systems is a key area of focus in MMF research. Current formulations of MMF, such as oral capsules and granules, have limitations in terms of bioavailability, patient compliance, and side effect profiles. These limitations have spurred research into alternative delivery systems, such as:
- Controlled-release formulations: These formulations aim to provide sustained and predictable levels of MMF in the body, potentially reducing the frequency of administration and improving patient compliance. For example, studies are investigating MMF formulations that release the drug gradually over a longer period, reducing the need for frequent dosing and minimizing fluctuations in drug levels.
- Targeted delivery systems: These systems aim to deliver MMF directly to the target tissues or organs, potentially enhancing efficacy and minimizing off-target effects. For instance, researchers are exploring the use of nanoparticles or liposomes to encapsulate MMF and deliver it specifically to the immune cells involved in transplant rejection or autoimmune disease. This approach could reduce systemic exposure to MMF and minimize adverse effects.
- Bioavailability enhancement strategies: These strategies aim to improve the absorption of MMF from the gastrointestinal tract, increasing its bioavailability and therapeutic efficacy. For example, researchers are investigating the use of co-formulations or novel excipients that can enhance MMF absorption and increase its bioavailability.
Improving Efficacy and Reducing Adverse Effects
Efforts to improve the efficacy and reduce the adverse effects of MMF involve:
- Optimizing dosing strategies: Research is ongoing to identify optimal dosing regimens for MMF, taking into account factors such as patient characteristics, disease severity, and individual drug metabolism. Personalized medicine approaches, which tailor dosing to individual patients, may help to improve efficacy and minimize adverse effects.
- Combinations with other immunosuppressants: Combining MMF with other immunosuppressants, such as calcineurin inhibitors or anti-proliferative agents, may offer synergistic effects and improve the efficacy of immunosuppression. For example, the combination of MMF with tacrolimus has shown promising results in reducing transplant rejection.
- Identifying biomarkers for therapeutic response: Identifying biomarkers that predict MMF response and toxicity could allow for personalized dosing and monitoring of therapy. Researchers are investigating biomarkers such as blood levels of MMF metabolites or genetic variations in drug-metabolizing enzymes.
Novel Therapeutic Strategies
Beyond its established role in immunosuppression, research is exploring novel therapeutic applications of MMF in various disease settings. These include:
- Cancer therapy: MMF’s immunosuppressive properties are being investigated in the context of cancer therapy, particularly in combination with other anticancer agents. MMF’s ability to suppress the immune response could potentially enhance the effectiveness of immunotherapy and reduce the incidence of graft-versus-host disease (GVHD) after bone marrow transplantation.
- Inflammatory bowel disease (IBD): MMF is showing promise in the treatment of IBD, where its anti-inflammatory properties may help to control inflammation and reduce disease activity. Research is exploring the use of MMF in combination with other IBD therapies, such as biologics, to improve outcomes.
- Neurological disorders: Emerging research suggests that MMF may have therapeutic potential in neurological disorders such as multiple sclerosis (MS). MMF’s ability to suppress the immune system may help to reduce inflammation and neurodegeneration in MS. Further research is needed to evaluate its safety and efficacy in these disorders.
Mycophenolate and Pregnancy
Mycophenolate, a powerful immunosuppressant medication, plays a crucial role in preventing organ rejection after transplantation and managing autoimmune diseases. However, its use during pregnancy presents a complex scenario, demanding careful consideration of both potential risks and benefits. This section delves into the intricate aspects of mycophenolate use during pregnancy, providing insights into its effects on fetal development, potential risks, and recommendations for managing pregnancy in patients receiving this medication.
Risks and Benefits of Mycophenolate Use During Pregnancy
Mycophenolate is classified as a pregnancy category D drug, indicating a proven risk of fetal harm. Studies have shown a significant association between mycophenolate exposure during pregnancy and various fetal abnormalities, including:
- Miscarriage: Studies have shown an increased risk of miscarriage in pregnant women exposed to mycophenolate. This risk is particularly elevated during the first trimester of pregnancy.
- Birth Defects: Mycophenolate can interfere with fetal development, leading to various birth defects. These defects can affect different organ systems, including the heart, brain, limbs, and urinary tract.
- Premature Birth: Mycophenolate exposure has been linked to an increased risk of premature birth, which can lead to complications for the newborn.
- Low Birth Weight: Infants born to mothers who took mycophenolate during pregnancy may have a lower birth weight than those not exposed to the drug.
Despite these risks, mycophenolate may be necessary to prevent organ rejection in transplant recipients or manage severe autoimmune diseases in some women. In such cases, the benefits of mycophenolate treatment may outweigh the potential risks to the fetus.
Managing Pregnancy in Patients Receiving Mycophenolate
Given the risks associated with mycophenolate use during pregnancy, it is crucial to carefully manage pregnancy in patients receiving this medication.
Recommendations for Management
- Preconception Counseling: Before attempting pregnancy, women receiving mycophenolate should undergo thorough preconception counseling with their healthcare provider. This counseling should include a comprehensive discussion of the potential risks and benefits of continuing mycophenolate treatment during pregnancy.
- Pregnancy Planning: If a woman decides to become pregnant while on mycophenolate, it is essential to plan the pregnancy carefully. This may involve adjusting the dosage or switching to an alternative immunosuppressant medication.
- Close Monitoring: Throughout pregnancy, women on mycophenolate should undergo close monitoring, including regular ultrasounds and fetal assessments. This allows healthcare providers to detect any potential problems with fetal development early on.
- Discontinuation of Mycophenolate: In many cases, it is recommended to discontinue mycophenolate as soon as possible after a positive pregnancy test. However, the decision to stop or continue mycophenolate treatment during pregnancy should be made on a case-by-case basis, taking into account the individual patient’s medical history, the severity of their condition, and the potential risks and benefits.
Potential Effects of Mycophenolate on Fetal Development
Mycophenolate’s potential to disrupt fetal development stems from its mechanism of action as an immunosuppressant. It inhibits the enzyme inosine monophosphate dehydrogenase (IMPDH), which is crucial for the synthesis of guanine nucleotides. These nucleotides are essential for DNA replication and cell division, processes vital for normal fetal growth and development.
Possible Effects
- Interference with DNA Synthesis: Mycophenolate’s inhibition of IMPDH can interfere with DNA synthesis in developing cells, potentially leading to developmental abnormalities.
- Cell Death: In some cases, mycophenolate can trigger cell death in developing tissues, contributing to birth defects.
- Immune System Development: Mycophenolate’s immunosuppressive effects can also impact the development of the fetal immune system, potentially increasing the risk of infections in the newborn.
The precise mechanisms by which mycophenolate affects fetal development are still being investigated. However, the available evidence suggests that its interference with DNA synthesis and cell division plays a significant role in its teratogenic potential.
Mycophenolate and Breastfeeding
Mycophenolate is a medication commonly used to suppress the immune system, particularly in organ transplant recipients and individuals with autoimmune diseases. While its effectiveness in these conditions is well-established, its use during breastfeeding raises concerns regarding potential risks to the infant. This section delves into the potential for mycophenolate excretion in breast milk, the associated risks and benefits of breastfeeding while taking mycophenolate, and provides guidance on alternative feeding options if necessary.
Potential for Excretion in Breast Milk
Mycophenolate is known to be excreted in breast milk. Studies have shown that the concentration of mycophenolate in breast milk is significantly lower than in maternal serum. However, the actual amount of mycophenolate transferred to the infant through breast milk can vary depending on factors such as the mother’s dosage, the infant’s age, and the time elapsed since the last dose.
Risks and Benefits of Breastfeeding
The decision to breastfeed while taking mycophenolate involves weighing the potential risks to the infant against the benefits of breastfeeding.
Potential Risks to the Infant
- Immune Suppression: Mycophenolate can suppress the infant’s immune system, making them more susceptible to infections. This risk is particularly relevant for infants with compromised immune systems or premature infants.
- Gastrointestinal Issues: Mycophenolate can cause gastrointestinal disturbances in infants, including diarrhea, vomiting, and abdominal pain.
- Long-Term Effects: The long-term effects of mycophenolate exposure in breastfed infants are not fully understood. However, there are concerns about potential developmental issues or increased risk of cancer in later life.
Benefits of Breastfeeding
- Nutritional Advantages: Breast milk provides optimal nutrition for infants, containing essential antibodies, vitamins, and minerals that support growth and development.
- Immune Protection: Breast milk provides passive immunity to the infant, protecting them from infections.
- Bonding and Emotional Benefits: Breastfeeding promotes bonding between mother and infant, contributing to emotional well-being.
Alternative Feeding Options
If the risks of breastfeeding outweigh the benefits, alternative feeding options should be considered. These include:
- Formula Feeding: Formula milk provides adequate nutrition for infants, although it lacks the immune-boosting properties of breast milk.
- Donor Milk: Donor milk from screened and healthy mothers can be a viable option for infants who cannot be breastfed.
Patient Education and Counseling
Mycophenolate is a medication that helps to suppress your body’s immune system. This is important because it prevents your body from rejecting a transplanted organ or attacking its own tissues in autoimmune diseases. It’s crucial to understand how this medication works, its potential benefits and risks, and how to take it properly.
Understanding Mycophenolate
Mycophenolate is a medication that works by suppressing your body’s immune system. This means it helps to prevent your body from rejecting a transplanted organ or attacking its own tissues in autoimmune diseases. It’s important to take mycophenolate exactly as your doctor prescribes it.
Benefits of Mycophenolate
Mycophenolate can help to:
- Prevent organ rejection after a transplant.
- Control symptoms of autoimmune diseases, such as lupus and rheumatoid arthritis.
Risks of Mycophenolate
Like all medications, mycophenolate can cause side effects. Some common side effects include:
- Diarrhea
- Nausea
- Vomiting
- Headache
- Stomach pain
More serious side effects can occur, but they are less common. These can include:
- Infection
- High blood pressure
- Kidney problems
- Low blood counts
It’s important to talk to your doctor if you experience any side effects, especially if they are severe or don’t go away.
Proper Use of Mycophenolate
- Take mycophenolate exactly as your doctor prescribes it.
- Do not miss doses.
- Do not stop taking mycophenolate without talking to your doctor.
- Store mycophenolate at room temperature, away from light and moisture.
Counseling Script for Healthcare Professionals
When discussing mycophenolate with patients, healthcare professionals should:
- Explain the purpose of mycophenolate and how it works.
- Discuss the potential benefits and risks of mycophenolate.
- Provide clear instructions on how to take mycophenolate.
- Answer any questions the patient may have.
- Encourage the patient to report any side effects they experience.
- Emphasize the importance of regular follow-up appointments.
Patient Information Sheet
Here are some common questions and concerns related to mycophenolate:
- What if I miss a dose of mycophenolate? If you miss a dose of mycophenolate, take it as soon as you remember. However, if it is almost time for your next dose, skip the missed dose and take your next dose at the regular time. Do not take a double dose to make up for a missed dose.
- What if I take too much mycophenolate? If you take too much mycophenolate, contact your doctor or poison control center immediately.
- Can I drink alcohol while taking mycophenolate? It’s best to avoid alcohol while taking mycophenolate, as it can increase the risk of side effects.
- Can I take other medications while taking mycophenolate? It’s important to tell your doctor about all the medications you are taking, including over-the-counter medications, vitamins, and herbal supplements. Some medications can interact with mycophenolate and increase the risk of side effects.
- Can I drive while taking mycophenolate? Mycophenolate can cause dizziness and drowsiness. If you experience these side effects, avoid driving or operating machinery.
- Can I get pregnant while taking mycophenolate? Mycophenolate can harm a developing fetus. If you are a woman of childbearing potential, you should use effective contraception while taking mycophenolate. It’s important to talk to your doctor about the risks and benefits of taking mycophenolate if you are pregnant or planning to become pregnant.
- Can I breastfeed while taking mycophenolate? Mycophenolate passes into breast milk and can harm a breastfeeding infant. It’s important to talk to your doctor about the risks and benefits of breastfeeding while taking mycophenolate.
Mycophenolate and Drug Interactions
Mycophenolate mofetil (MMF) is a commonly used immunosuppressant medication, particularly in the context of organ transplantation and autoimmune diseases. Its effectiveness in preventing organ rejection and managing autoimmune conditions is well-established. However, the therapeutic efficacy of MMF can be influenced by interactions with other medications, potentially leading to altered drug levels, decreased efficacy, or increased risk of adverse effects. This section explores the potential interactions of MMF with other medications, elucidates the mechanisms underlying these interactions, and provides recommendations for managing drug interactions to optimize MMF efficacy and minimize adverse events.
Drug Interactions with Mycophenolate
Drug interactions with MMF can occur due to various mechanisms, including:
- Pharmacokinetic Interactions: These interactions involve alterations in the absorption, distribution, metabolism, or elimination of MMF, resulting in changes in its plasma concentrations.
- Pharmacodynamic Interactions: These interactions occur when MMF and another drug affect the same physiological pathway or target, leading to either additive or antagonistic effects.
Pharmacokinetic Interactions
Pharmacokinetic interactions can significantly impact MMF levels and efficacy. These interactions are often categorized based on their impact on the absorption, metabolism, or elimination of MMF.
- Absorption: Some medications, such as antacids, can reduce the absorption of MMF by altering the gastric pH or binding to the drug in the gastrointestinal tract. For instance, the administration of MMF with antacids like aluminum hydroxide or magnesium hydroxide can significantly decrease its absorption.
- Metabolism: MMF is primarily metabolized by the enzyme inosine monophosphate dehydrogenase (IMPDH), which is responsible for the synthesis of guanine nucleotides. Medications that inhibit or induce IMPDH activity can influence the metabolism of MMF, leading to changes in its plasma levels. For example, azathioprine, another immunosuppressant, can compete with MMF for metabolism by IMPDH, potentially increasing MMF levels. Conversely, drugs that induce IMPDH activity, such as rifampicin, may accelerate MMF metabolism, resulting in lower plasma levels.
- Elimination: MMF is primarily eliminated through the kidneys. Medications that affect renal function, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or aminoglycoside antibiotics, can impair MMF elimination, leading to increased drug accumulation and potential toxicity.
Pharmacodynamic Interactions
Pharmacodynamic interactions occur when MMF and another drug affect the same physiological pathway or target, leading to either additive or antagonistic effects.
- Additive Effects: When two drugs with similar mechanisms of action are used concurrently, their effects can be additive. For example, the combination of MMF with other immunosuppressants, such as cyclosporine or tacrolimus, can enhance the immunosuppressive effect but also increase the risk of adverse effects.
- Antagonistic Effects: Conversely, some drugs can antagonize the effects of MMF. For example, certain antivirals, such as ganciclovir, can interfere with the immunosuppressive activity of MMF, potentially reducing its efficacy.
Managing Drug Interactions
Managing drug interactions with MMF is crucial to ensure optimal efficacy and minimize adverse events.
- Monitoring: Regular monitoring of MMF plasma levels is essential, especially when co-administered with other medications that can interact with it. Monitoring allows for timely adjustments in dosage or drug selection to maintain therapeutic levels and minimize the risk of toxicity.
- Dosage Adjustments: Dosage adjustments may be necessary when MMF is co-administered with interacting medications. For example, the dosage of MMF may need to be reduced when co-administered with drugs that inhibit its metabolism or increase its plasma levels. Conversely, the dosage may need to be increased when co-administered with drugs that induce its metabolism or decrease its plasma levels.
- Alternative Medications: In some cases, alternative medications with fewer drug interactions may be considered if the risk of interaction with MMF is significant. However, this decision should be made on a case-by-case basis, taking into account the patient’s individual needs and the potential benefits and risks of alternative medications.
- Timing of Administration: In some cases, adjusting the timing of administration of MMF and other medications can minimize the risk of interaction. For example, administering MMF with food can increase its absorption, potentially reducing the impact of medications that interfere with its absorption.
Examples of Drug Interactions
Here are some specific examples of drug interactions with MMF:
| Drug | Mechanism of Interaction | Potential Effects | Management |
|---|---|---|---|
| Antacids (aluminum hydroxide, magnesium hydroxide) | Decreased absorption of MMF | Reduced MMF levels, decreased efficacy | Administer MMF at least 2 hours before or 4 hours after antacids |
| Azathioprine | Competition for metabolism by IMPDH | Increased MMF levels, increased risk of toxicity | Monitor MMF levels closely, adjust dosage as needed |
| Rifampicin | Induction of IMPDH activity | Decreased MMF levels, decreased efficacy | Monitor MMF levels closely, adjust dosage as needed |
| Nonsteroidal anti-inflammatory drugs (NSAIDs) | Impaired renal function | Increased MMF levels, increased risk of toxicity | Monitor renal function closely, adjust dosage as needed |
| Aminoglycoside antibiotics | Impaired renal function | Increased MMF levels, increased risk of toxicity | Monitor renal function closely, adjust dosage as needed |
| Cyclosporine, tacrolimus | Additive immunosuppressive effects | Increased risk of adverse effects | Monitor for signs of toxicity, adjust dosages as needed |
| Ganciclovir | Antagonism of MMF’s immunosuppressive effects | Decreased efficacy of MMF | Consider alternative antiviral agents |
Conclusion
MMF is an effective immunosuppressant, but its efficacy can be influenced by interactions with other medications. Understanding the mechanisms underlying these interactions and implementing appropriate management strategies are crucial to optimize MMF efficacy and minimize adverse events. Regular monitoring of MMF plasma levels, dosage adjustments, and consideration of alternative medications or timing of administration can help mitigate the potential risks associated with drug interactions.
Mycophenolate’s impact on the field of medicine is undeniable. Its ability to modulate the immune system has provided hope for patients facing organ rejection and autoimmune disorders. However, as with any powerful medication, understanding its potential adverse effects and proper use is crucial. Through careful monitoring and patient education, healthcare professionals can maximize the benefits of mycophenolate while minimizing risks, ensuring optimal patient outcomes.
Mycophenolate is a powerful immunosuppressant often used to prevent organ rejection after transplantation. While its primary focus is on the immune system, it’s important to consider the potential interactions with other medications. For instance, mycophenolate can interact with drugs like atorvastatin , a common cholesterol-lowering medication. Understanding these interactions is crucial for managing the overall health of transplant patients.