Oxaliplatin, a platinum-based chemotherapy drug, stands as a powerful weapon in the fight against cancer. Its unique mechanism of action targets DNA synthesis, disrupting the rapid cell division that characterizes cancerous growth. Oxaliplatin has proven effective in treating a range of cancers, particularly those of the gastrointestinal tract, and its use continues to evolve with ongoing research.
This complex molecule, often administered intravenously, plays a crucial role in both primary and adjuvant cancer therapies. Its effectiveness is often enhanced when combined with other chemotherapy agents or targeted therapies, creating potent regimens designed to combat the disease from multiple angles. While offering hope, oxaliplatin’s journey is not without challenges. Like many cancer treatments, it can cause side effects, ranging from manageable to severe. Understanding these side effects and implementing effective management strategies is essential for maximizing the benefits of this potent drug.
Oxaliplatin
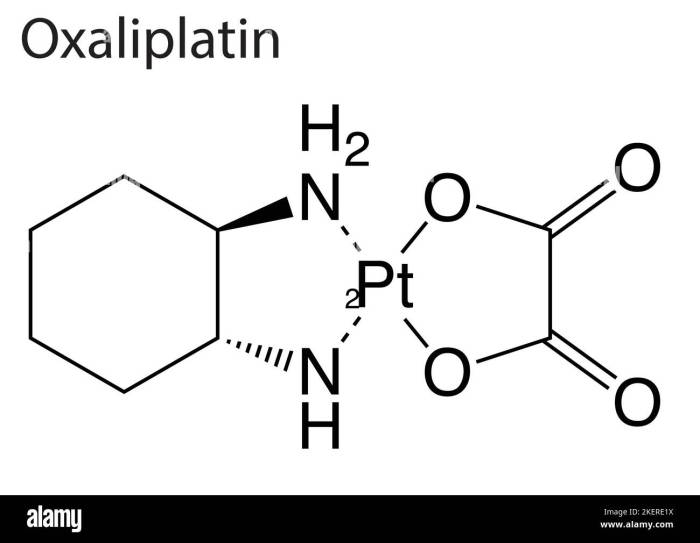
Oxaliplatin is a chemotherapy drug used to treat various types of cancer. It is a platinum-based drug, meaning it contains platinum in its chemical structure. The chemical formula for oxaliplatin is (1R,2R)-1,2-cyclohexanediamineplatinum(II) dichloride. It is classified as an antineoplastic agent, which means it inhibits the growth and spread of cancer cells.
Mechanism of Action
Oxaliplatin works by interfering with DNA synthesis and cell division. When oxaliplatin enters the body, it binds to DNA, forming platinum-DNA adducts. These adducts prevent DNA from replicating properly, leading to cell death. Oxaliplatin also induces apoptosis, a process of programmed cell death.
Role in Cancer Treatment
Oxaliplatin is used to treat various types of cancer, including:
- Colorectal cancer: Oxaliplatin is a mainstay in the treatment of colorectal cancer, often used in combination with other chemotherapy drugs like 5-fluorouracil (5-FU) and leucovorin.
- Gastric cancer: Oxaliplatin can be used in combination with other chemotherapy drugs to treat gastric cancer, particularly in advanced stages.
- Ovarian cancer: Oxaliplatin is sometimes used in combination with other drugs to treat ovarian cancer, especially in patients with platinum-sensitive tumors.
- Lung cancer: Oxaliplatin is used in combination with other chemotherapy drugs to treat non-small cell lung cancer, particularly in patients with specific genetic mutations.
Oxaliplatin’s effectiveness in treating cancer varies depending on the type and stage of the cancer, as well as the patient’s individual characteristics. It is important to note that oxaliplatin can have significant side effects, including nausea, vomiting, diarrhea, neuropathy, and bone marrow suppression.
Clinical Applications of Oxaliplatin
Oxaliplatin, a platinum-based chemotherapy drug, has a significant role in treating various types of cancer. Its effectiveness stems from its ability to interfere with DNA replication, ultimately leading to cancer cell death.
Common Cancers Treated with Oxaliplatin
Oxaliplatin is commonly used in the treatment of several types of cancer, both as a primary and adjuvant therapy. Here’s a breakdown:
- Colorectal Cancer: Oxaliplatin is a cornerstone treatment for advanced colorectal cancer, often used in combination with other chemotherapy drugs like 5-fluorouracil (5-FU) and leucovorin. It is also used as an adjuvant therapy after surgery to reduce the risk of cancer recurrence.
- Gastric Cancer: Oxaliplatin can be used in combination with other chemotherapy agents to treat advanced gastric cancer.
- Ovarian Cancer: Oxaliplatin is sometimes used in combination with other chemotherapy drugs to treat advanced ovarian cancer.
- Esophageal Cancer: Oxaliplatin can be used in combination with other chemotherapy agents to treat advanced esophageal cancer.
- Pancreatic Cancer: Oxaliplatin is sometimes used in combination with other chemotherapy drugs to treat advanced pancreatic cancer.
Dosage and Administration
The dosage and administration of oxaliplatin vary depending on the type of cancer being treated, the patient’s overall health, and other factors. The most common administration route is intravenous (IV) infusion.
Typical dosages range from 85 to 130 mg/m2, administered every 2 to 3 weeks.
Common Regimens Involving Oxaliplatin
Oxaliplatin is often used in combination with other chemotherapy drugs or targeted therapies. Here are some common regimens:
| Regimen Name | Drugs | Indications |
|---|---|---|
| FOLFOX | Oxaliplatin, 5-FU, leucovorin | Advanced colorectal cancer |
| XELOX | Oxaliplatin, capecitabine | Advanced colorectal cancer |
| FOLFIRI | Oxaliplatin, irinotecan, 5-FU, leucovorin | Advanced colorectal cancer |
| mFOLFOX6 | Oxaliplatin, 5-FU, leucovorin, bevacizumab | Advanced colorectal cancer |
Side Effects and Toxicity: Oxaliplatin
Oxaliplatin, while effective in treating various cancers, can cause a range of side effects. These side effects can vary in severity and duration, and understanding them is crucial for effective management and patient well-being.
Acute Side Effects
Acute side effects are those that occur during or shortly after oxaliplatin administration.
- Nausea and Vomiting: This is a common side effect, often occurring within a few hours of treatment. Anti-nausea medications, such as ondansetron or granisetron, can be administered to prevent or alleviate these symptoms.
- Diarrhea: Some patients may experience diarrhea, which can be mild or severe. Medications like loperamide can help manage this side effect.
- Peripheral Neuropathy: This refers to nerve damage, particularly affecting the hands and feet. It can manifest as tingling, numbness, or weakness. This side effect can be dose-dependent and can sometimes persist even after treatment ends.
- Myelosuppression: Oxaliplatin can suppress bone marrow function, leading to a decrease in blood cell counts. This can increase the risk of infections and bleeding.
- Hypersensitivity Reactions: In rare cases, patients may experience allergic reactions to oxaliplatin, which can range from mild skin rashes to severe anaphylaxis.
Management of Acute Side Effects
Managing acute side effects is crucial for patient comfort and adherence to treatment.
- Pre-medication: Anti-nausea medications and antihistamines can be administered before oxaliplatin treatment to reduce the risk of nausea, vomiting, and allergic reactions.
- Supportive Care: This includes adequate hydration, pain management, and monitoring of vital signs. Blood transfusions may be necessary in cases of severe myelosuppression.
- Dose Adjustment: If side effects are severe, the dose of oxaliplatin may need to be adjusted or treatment may be temporarily paused.
Long-Term Side Effects
Long-term side effects can occur weeks, months, or even years after oxaliplatin treatment has ended.
- Peripheral Neuropathy: This can persist or worsen over time, leading to difficulty with fine motor skills and daily activities.
- Hearing Loss: Some patients may experience hearing loss, particularly at high frequencies.
- Cognitive Impairment: In some cases, oxaliplatin can lead to cognitive difficulties, including memory problems and difficulty concentrating.
- Cardiotoxicity: Although rare, oxaliplatin can potentially affect heart function, leading to heart failure or arrhythmias.
- Secondary Malignancies: Long-term exposure to oxaliplatin may increase the risk of developing secondary cancers.
Patient Experiences
The severity and duration of oxaliplatin side effects can vary widely among patients.
“I experienced severe nausea and vomiting during my first few cycles of oxaliplatin. It was debilitating, but the anti-nausea medication helped manage it. The neuropathy was more challenging, as it persisted even after treatment ended. I had to adapt to my limitations, but I am grateful for the treatment’s effectiveness.” – Sarah, a breast cancer survivor
“I was fortunate to experience minimal side effects from oxaliplatin. I had some mild fatigue and occasional tingling in my fingers, but it was manageable. I am thankful for the treatment’s success and the minimal impact on my quality of life.” – David, a colorectal cancer survivor
Resistance and Mechanisms of Resistance
Oxaliplatin resistance is a significant obstacle in the treatment of colorectal cancer. It can lead to tumor recurrence and poor patient outcomes. This phenomenon arises from complex mechanisms that involve various molecular pathways. Understanding these mechanisms is crucial for developing strategies to overcome resistance and improve therapeutic efficacy.
Molecular Mechanisms of Oxaliplatin Resistance
The development of oxaliplatin resistance involves multiple cellular mechanisms that enable cancer cells to evade the cytotoxic effects of the drug. These mechanisms can be broadly classified into:
- Altered Drug Uptake and Efflux: Cancer cells can develop mechanisms to reduce the intracellular concentration of oxaliplatin. This can occur through decreased drug uptake or increased drug efflux.
- DNA Repair Pathways: Oxaliplatin primarily exerts its cytotoxic effects by inducing DNA damage. Cancer cells can become resistant by upregulating DNA repair pathways, such as nucleotide excision repair (NER) and mismatch repair (MMR), which effectively remove the DNA lesions caused by oxaliplatin.
- Changes in Drug Targets: Oxaliplatin exerts its cytotoxic effects by binding to DNA and inducing DNA damage. Mutations in the DNA binding site or other proteins involved in DNA replication can lead to resistance by reducing the drug’s ability to bind to its target.
- Altered Apoptosis Signaling Pathways: Apoptosis is a programmed cell death pathway that is triggered by oxaliplatin. Cancer cells can become resistant by dysregulating apoptosis signaling pathways, such as the p53 pathway or the caspase cascade, leading to reduced cell death.
- Increased Drug Detoxification: Cancer cells can enhance their ability to detoxify oxaliplatin through the upregulation of drug-metabolizing enzymes, such as glutathione S-transferases (GSTs). These enzymes can conjugate oxaliplatin with glutathione, making it less toxic and facilitating its excretion.
Strategies to Overcome Oxaliplatin Resistance
Overcoming oxaliplatin resistance is a challenging task that requires a multi-pronged approach. Strategies to overcome resistance include:
- Combination Therapies: Combining oxaliplatin with other chemotherapeutic agents that target different pathways or have different mechanisms of action can help overcome resistance. For example, combining oxaliplatin with 5-fluorouracil (5-FU) or irinotecan can enhance anti-tumor activity and reduce the development of resistance.
- Targeted Therapies: Targeting specific molecular pathways involved in oxaliplatin resistance can help restore drug sensitivity. For example, inhibiting DNA repair pathways or targeting drug efflux pumps can enhance the effectiveness of oxaliplatin.
- Drug Delivery Strategies: Novel drug delivery systems, such as nanoparticles or liposomes, can be used to improve the delivery of oxaliplatin to tumor cells and circumvent resistance mechanisms.
- Development of New Drugs: Developing new platinum-based drugs with different mechanisms of action or non-platinum-based drugs that target the same pathways as oxaliplatin can help overcome resistance.
Future Directions in Oxaliplatin Research
Despite its significant contributions to cancer treatment, oxaliplatin research continues to explore ways to enhance its efficacy and mitigate its side effects. Ongoing research focuses on optimizing therapy through personalized medicine approaches, exploring novel combinations with other therapies, and investigating potential new applications.
Personalized Medicine Approaches
Personalized medicine aims to tailor treatment strategies to individual patients based on their unique genetic and molecular profiles. This approach can help optimize oxaliplatin therapy by:
- Predicting Response: Identifying biomarkers that predict patient response to oxaliplatin can help select patients who are most likely to benefit from the treatment. For instance, research is exploring the role of genes involved in drug metabolism and DNA repair pathways in predicting oxaliplatin sensitivity.
- Optimizing Dosage: Genetic variations in drug metabolism can influence how patients process and eliminate oxaliplatin. Personalized dosing strategies based on individual genetic profiles can help minimize side effects and maximize therapeutic efficacy.
- Targeting Resistance: Understanding the molecular mechanisms of oxaliplatin resistance can lead to the development of targeted therapies to overcome resistance and restore sensitivity to the drug. For example, research is exploring the use of inhibitors that target specific proteins involved in oxaliplatin resistance pathways.
Combination Therapies
Combining oxaliplatin with other therapies can potentially enhance its effectiveness and broaden its therapeutic applications. Current research focuses on combining oxaliplatin with:
- Immunotherapy: Combining oxaliplatin with immunotherapy drugs, such as checkpoint inhibitors, can boost the immune system’s ability to target and destroy cancer cells. This approach has shown promising results in treating certain types of cancer, including colorectal cancer.
- Gene Therapy: Gene therapy approaches aim to modify the genetic makeup of cancer cells to make them more susceptible to oxaliplatin treatment. For example, research is exploring the use of gene therapy to deliver genes that enhance the sensitivity of cancer cells to oxaliplatin.
- Targeted Therapies: Combining oxaliplatin with targeted therapies that inhibit specific signaling pathways involved in cancer cell growth and survival can potentially enhance its effectiveness. This approach has been explored in clinical trials for various cancers, including colorectal and pancreatic cancer.
Promising Research Areas
Ongoing research is exploring various aspects of oxaliplatin, aiming to improve its therapeutic profile and expand its applications. Key areas of focus include:
- Drug Development: Researchers are exploring new formulations and delivery methods for oxaliplatin to improve its bioavailability, reduce side effects, and enhance its efficacy. For example, nanotechnology-based drug delivery systems are being investigated to target oxaliplatin specifically to tumor cells.
- Resistance Mechanisms: Understanding the mechanisms of oxaliplatin resistance is crucial for developing strategies to overcome it. Research is focused on identifying the molecular pathways involved in resistance and developing targeted therapies to reverse resistance.
- Clinical Trial Designs: Innovative clinical trial designs are being implemented to evaluate the efficacy and safety of oxaliplatin in different patient populations and in combination with other therapies. These designs aim to optimize the selection of patients who are most likely to benefit from oxaliplatin treatment and to identify the most effective treatment combinations.
Oxaliplatin and Quality of Life
Oxaliplatin, while effective in treating certain cancers, can significantly impact patients’ quality of life due to its side effects. These effects can range from manageable discomfort to severe complications, influencing patients’ physical, emotional, and social well-being. Understanding the impact of oxaliplatin on quality of life is crucial for providing comprehensive care and support to patients undergoing this treatment.
Impact of Oxaliplatin on Quality of Life
Oxaliplatin’s impact on quality of life is multifaceted, encompassing various aspects of daily living.
- Fatigue: A common side effect, fatigue can significantly limit patients’ ability to perform daily activities, work, or participate in social events. This can lead to feelings of frustration, isolation, and decreased overall well-being.
- Nausea and Vomiting: These gastrointestinal side effects can be debilitating, impacting patients’ appetite, nutritional intake, and overall comfort. Nausea and vomiting can lead to dehydration, weight loss, and reduced quality of life.
- Cognitive Impairment: Some patients experience cognitive impairment, commonly referred to as “chemo brain,” which can affect memory, concentration, and decision-making. This can impact patients’ work, social interactions, and overall cognitive function.
- Peripheral Neuropathy: A significant side effect, peripheral neuropathy causes numbness, tingling, and pain in the hands and feet. This can interfere with daily activities, such as writing, typing, or walking, impacting patients’ independence and quality of life.
- Emotional Distress: The diagnosis of cancer and the experience of treatment can cause emotional distress, including anxiety, depression, and fear. This can significantly impact patients’ quality of life, affecting their relationships and overall well-being.
Strategies to Improve Quality of Life
Various strategies can help improve quality of life during and after oxaliplatin therapy:
- Supportive Care: Healthcare professionals play a vital role in providing supportive care, including medication to manage nausea and vomiting, physical therapy to address neuropathy, and counseling to address emotional distress.
- Lifestyle Modifications: Patients can adopt lifestyle modifications to improve their well-being, such as eating a healthy diet, staying hydrated, getting regular exercise, and getting enough sleep.
- Counseling: Counseling can help patients cope with the emotional and psychological challenges associated with cancer treatment, including anxiety, depression, and fear. It can provide patients with strategies for managing stress, improving coping skills, and maintaining a positive outlook.
- Support Groups: Connecting with others who have similar experiences can provide emotional support, practical advice, and a sense of community. Support groups offer a safe space for patients to share their experiences, ask questions, and learn from others.
Patient Narratives
- Example 1: “The fatigue was the hardest part. I couldn’t do the things I used to love, like going for walks or spending time with my grandchildren. It felt like I was constantly dragging myself through the day.” – Sarah, a breast cancer patient who underwent oxaliplatin treatment.
- Example 2: “The neuropathy was really difficult. I couldn’t hold a pen to write, and I had trouble walking. It made me feel so helpless and frustrated.” – David, a colon cancer patient who received oxaliplatin therapy.
- Example 3: “Talking to a therapist really helped me cope with the emotional stress of treatment. It gave me a safe space to process my feelings and learn strategies for managing anxiety and depression.” – Maria, an ovarian cancer patient who underwent oxaliplatin treatment.
Oxaliplatin and the Future of Cancer Treatment
Oxaliplatin, a platinum-based chemotherapy drug, has played a significant role in the treatment of various cancers, particularly colorectal cancer. Its effectiveness has been well-established, but ongoing research continues to explore its potential in the evolving landscape of cancer treatment.
Oxaliplatin in Combination Therapies
The use of oxaliplatin in combination with other therapies holds significant promise for enhancing treatment outcomes. Combining oxaliplatin with other chemotherapy agents, targeted therapies, or immunotherapy drugs can potentially synergize their effects, leading to improved tumor response and patient survival. For example, combining oxaliplatin with bevacizumab, a vascular endothelial growth factor (VEGF) inhibitor, has been shown to improve progression-free survival in patients with metastatic colorectal cancer.
Oxaliplatin and Emerging Technologies
Oxaliplatin’s future potential extends to its integration with emerging technologies like nanomedicine and precision medicine.
- Nanomedicine involves the use of nanoparticles to deliver drugs more effectively and target specific cancer cells. This approach could enhance the efficacy of oxaliplatin while minimizing side effects. For instance, encapsulating oxaliplatin in nanoparticles could improve its penetration into tumors and prolong its release, leading to sustained drug levels in the tumor microenvironment.
- Precision medicine aims to personalize cancer treatment based on an individual’s genetic makeup. By identifying specific genetic alterations that drive tumor growth, researchers can develop targeted therapies that are more effective and have fewer side effects. Oxaliplatin could be used in combination with precision medicine approaches to tailor treatment to individual patients. For example, patients with specific genetic mutations that predict sensitivity to oxaliplatin could benefit from receiving this drug as part of their personalized treatment plan.
Long-Term Implications of Oxaliplatin Research
The continued research into oxaliplatin has the potential to significantly impact the fight against cancer.
- Developing new formulations and delivery methods could improve the drug’s efficacy and reduce its side effects.
- Investigating oxaliplatin’s mechanisms of action could lead to the development of new drugs with similar or enhanced therapeutic properties.
- Exploring the combination of oxaliplatin with other therapies could revolutionize cancer treatment strategies, offering patients more effective and personalized treatment options.
Oxaliplatin’s story is one of scientific innovation and clinical progress. Its ability to disrupt DNA synthesis and inhibit cell division has made it a valuable tool in the fight against cancer. However, the journey to harness its full potential is ongoing, with researchers exploring new combinations, targeted delivery methods, and personalized approaches. As our understanding of this complex drug deepens, we move closer to a future where cancer treatments are more effective, targeted, and less burdensome for patients.
Oxaliplatin, a chemotherapy drug used to treat certain types of cancer, can sometimes have side effects on the heart. While not directly related, it’s interesting to note that cardiac glycosides, a class of drugs that have been used to treat heart conditions for centuries, can also have a significant impact on heart function. Understanding the potential effects of oxaliplatin on the heart is crucial for monitoring and managing patient care.