Risperidone, a powerful atypical antipsychotic, has revolutionized the treatment of mental health conditions. This medication, often prescribed for schizophrenia and bipolar disorder, works by regulating neurotransmitters in the brain, ultimately helping to alleviate symptoms like hallucinations and delusions. But understanding risperidone goes beyond its clinical applications; it delves into its complex mechanism of action, potential side effects, and ethical considerations surrounding its use.
This exploration will provide a comprehensive overview of risperidone, examining its chemical structure, therapeutic applications, pharmacokinetic properties, and potential adverse effects. We will also discuss important aspects like dosage, administration, and monitoring, along with the ethical implications of its use. By understanding the multifaceted nature of risperidone, we can better appreciate its role in improving the lives of those who struggle with mental illness.
Risperidone
Risperidone is an atypical antipsychotic medication used to treat schizophrenia and bipolar disorder. It is also used to treat agitation and aggression in people with dementia. Risperidone works by blocking dopamine and serotonin receptors in the brain. This helps to reduce the symptoms of psychosis, such as hallucinations and delusions.
Chemical Structure and Properties
Risperidone is a white to off-white crystalline powder that is soluble in water. Its chemical formula is C23H27N3O2, and its molecular weight is 381.5 g/mol. Risperidone is a selective antagonist of dopamine D2 and serotonin 5-HT2A receptors.
Mechanism of Action
Risperidone works by blocking dopamine and serotonin receptors in the brain. This helps to reduce the symptoms of psychosis, such as hallucinations and delusions. Risperidone is an atypical antipsychotic, meaning that it has a higher affinity for serotonin receptors than for dopamine receptors. This difference in affinity is thought to be responsible for some of the unique effects of risperidone, such as its lower risk of extrapyramidal side effects.
Pharmacological Effects
Risperidone has a variety of pharmacological effects, including:
- Antipsychotic effects: Risperidone blocks dopamine receptors in the mesolimbic pathway, which is thought to be involved in the development of psychosis. This helps to reduce the symptoms of psychosis, such as hallucinations and delusions.
- Anxiolytic effects: Risperidone has been shown to reduce anxiety in some people. This may be due to its effects on serotonin receptors in the brain.
- Antidepressant effects: Risperidone has been shown to improve mood in some people with depression. This may be due to its effects on dopamine and serotonin receptors in the brain.
- Anti-emetic effects: Risperidone has been shown to reduce nausea and vomiting in some people. This may be due to its effects on dopamine receptors in the chemoreceptor trigger zone (CTZ) of the brain.
Therapeutic Applications of Risperidone
Risperidone is a widely used antipsychotic medication with a broad range of therapeutic applications. It is primarily prescribed for managing psychotic disorders, but its effectiveness extends to treating other mental health conditions.
Schizophrenia and Other Psychotic Disorders
Risperidone is a first-line treatment option for schizophrenia and other psychotic disorders. It effectively alleviates the positive symptoms of psychosis, such as hallucinations and delusions, and also helps manage negative symptoms, including social withdrawal and apathy. Risperidone works by blocking dopamine receptors in the brain, which helps regulate neurotransmission and reduce the severity of psychotic symptoms.
Bipolar Disorder and Other Mood Disorders
Risperidone is also used in the management of bipolar disorder, particularly during manic episodes. It helps stabilize mood swings and reduce the intensity of manic symptoms, such as increased energy, racing thoughts, and impulsivity. Risperidone can be used in combination with other mood stabilizers, such as lithium or valproic acid, to achieve optimal treatment outcomes. In addition, risperidone has been found to be effective in treating other mood disorders, such as major depressive disorder, when used in conjunction with other antidepressants.
Pharmacokinetics and Metabolism of Risperidone
Risperidone’s pharmacokinetic profile, encompassing its absorption, distribution, metabolism, and excretion, is crucial in understanding its therapeutic effects and potential adverse events. This section delves into these aspects, highlighting factors influencing its pharmacokinetic behavior and comparing it to other atypical antipsychotics.
Absorption
Risperidone is rapidly absorbed after oral administration, with peak plasma concentrations typically reached within 1-2 hours. The bioavailability of risperidone is approximately 70%, meaning about 70% of the administered dose reaches the systemic circulation. Food does not significantly affect the rate or extent of absorption.
Distribution
Risperidone is highly bound to plasma proteins, primarily albumin. It distributes extensively to various tissues, including the brain, liver, and kidneys.
Metabolism
Risperidone is extensively metabolized in the liver, primarily by CYP2D6 and CYP3A4 enzymes. The primary metabolic pathway involves hydroxylation, resulting in the formation of paliperidone, which is also pharmacologically active.
Excretion
Risperidone and its active metabolite, paliperidone, are primarily excreted in the urine, with a smaller amount excreted in the feces. The elimination half-life of risperidone is approximately 3 hours, while that of paliperidone is approximately 24 hours.
Factors Influencing Pharmacokinetics
Several factors can influence the pharmacokinetic profile of risperidone, including:
- Age: Elderly patients may have a slower metabolism and elimination of risperidone, potentially leading to higher drug levels and an increased risk of side effects.
- Renal Function: Patients with impaired renal function may experience slower elimination of risperidone and its metabolites, leading to accumulation and increased risk of adverse effects.
- Hepatic Function: Patients with impaired hepatic function may have reduced metabolism of risperidone, resulting in higher drug levels and an increased risk of adverse effects.
- Genetic Factors: Genetic variations in CYP2D6 and CYP3A4 enzymes can influence the metabolism of risperidone. Individuals with reduced activity of these enzymes may experience higher drug levels.
- Concomitant Medications: Co-administration of risperidone with other drugs that inhibit CYP2D6 or CYP3A4 enzymes can lead to increased risperidone levels and an increased risk of adverse effects.
Comparison with Other Atypical Antipsychotics, Risperidone
Risperidone’s pharmacokinetic profile is similar to other atypical antipsychotics in terms of absorption, distribution, and protein binding. However, there are differences in their metabolism and elimination. For example, olanzapine has a longer elimination half-life than risperidone, while quetiapine has a faster elimination rate.
Risperidone’s pharmacokinetic profile is influenced by various factors, including age, renal function, hepatic function, genetic variations, and concomitant medications. It is essential to consider these factors when prescribing risperidone to optimize its therapeutic effects and minimize potential adverse events.
Adverse Effects and Drug Interactions
Risperidone, like other antipsychotics, can cause a range of adverse effects, some of which can be serious. Understanding these potential side effects and how to manage them is crucial for safe and effective treatment. Additionally, risperidone can interact with other medications, potentially leading to increased or decreased drug effects. This section will discuss the common and serious adverse effects associated with risperidone use, potential drug interactions, and strategies for managing adverse effects and minimizing drug interactions.
Common Adverse Effects
Common adverse effects of risperidone are generally mild and tend to improve over time. These include:
- Extrapyramidal Symptoms (EPS): These are movement disorders that can include muscle stiffness, tremors, restlessness, and involuntary movements. These symptoms are more common in older adults and those with a history of EPS.
- Sedation: Drowsiness and fatigue are common side effects, especially during the initial stages of treatment.
- Weight Gain: Risperidone can lead to weight gain, particularly in the long term.
- Metabolic Changes: Risperidone can increase blood sugar levels, cholesterol, and triglycerides.
- Prolactin Elevation: Risperidone can increase prolactin levels, which can lead to breast enlargement, milk production, and menstrual irregularities.
- Orthostatic Hypotension: Risperidone can cause a drop in blood pressure upon standing, leading to dizziness and lightheadedness.
- Anticholinergic Effects: Dry mouth, blurred vision, constipation, and urinary retention are possible side effects.
Serious Adverse Effects
While less common, risperidone can cause serious adverse effects that require immediate medical attention. These include:
- Neuroleptic Malignant Syndrome (NMS): A rare but life-threatening condition characterized by high fever, muscle rigidity, altered mental status, and autonomic instability.
- Tardive Dyskinesia (TD): A movement disorder that involves involuntary, repetitive movements of the face, tongue, and limbs. It can be irreversible in some cases.
- QT Prolongation: Risperidone can prolong the QT interval on an electrocardiogram (ECG), increasing the risk of potentially fatal heart rhythm abnormalities.
- Cerebrovascular Events: Risperidone has been associated with an increased risk of stroke, especially in older adults.
- Suicidal Thoughts and Behaviors: Antipsychotics, including risperidone, can increase the risk of suicidal thoughts and behaviors, particularly in young adults.
Drug Interactions
Risperidone can interact with various medications, potentially affecting their effectiveness or increasing the risk of side effects. Some important drug interactions include:
- Central Nervous System Depressants: Combining risperidone with other medications that depress the central nervous system, such as benzodiazepines, opioids, and alcohol, can increase the risk of sedation, dizziness, and respiratory depression.
- Anticholinergics: Risperidone’s anticholinergic effects can be exacerbated by other anticholinergic medications, increasing the risk of dry mouth, constipation, and urinary retention.
- Drugs That Prolong the QT Interval: Combining risperidone with other drugs that prolong the QT interval, such as certain antibiotics and antiarrhythmics, can increase the risk of potentially fatal heart rhythm abnormalities.
- CYP3A4 Inhibitors: Medications that inhibit the CYP3A4 enzyme, such as ketoconazole and erythromycin, can increase risperidone levels in the body, potentially leading to increased side effects.
- CYP3A4 Inducers: Medications that induce the CYP3A4 enzyme, such as carbamazepine and rifampin, can decrease risperidone levels in the body, potentially reducing its effectiveness.
Managing Adverse Effects and Minimizing Drug Interactions
- Monitoring and Management: Regular monitoring of vital signs, blood sugar levels, and prolactin levels is essential to detect and manage potential adverse effects.
- Dose Adjustment: The dose of risperidone may need to be adjusted to minimize side effects or optimize treatment effectiveness.
- Lifestyle Modifications: Lifestyle modifications, such as regular exercise, a healthy diet, and weight management, can help mitigate some adverse effects, such as weight gain and metabolic changes.
- Drug Interaction Considerations: It is crucial to inform healthcare providers about all medications, including over-the-counter drugs, herbal supplements, and vitamins, to minimize the risk of drug interactions.
Dosage and Administration of Risperidone
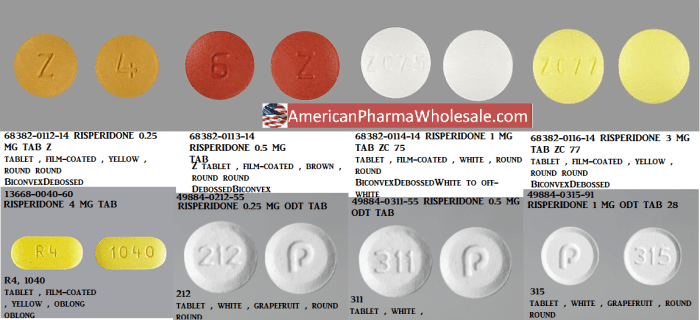
Risperidone is available in various formulations, including tablets, oral solution, and injectable forms. The recommended dosage and administration route depend on the specific condition being treated and the individual patient’s needs.
Dosage Adjustment Based on Individual Patient Factors
Dosage adjustment is crucial for optimizing therapeutic effects and minimizing adverse events. Factors influencing dosage include age, weight, renal and hepatic function, and the severity of the condition being treated.
- Age: Elderly patients may require lower doses due to increased sensitivity to risperidone’s effects.
- Weight: Individuals with lower body weight may require lower doses to achieve the desired therapeutic effect.
- Renal Function: Patients with impaired renal function may need dose adjustments to avoid accumulation of the drug in the body.
- Hepatic Function: Patients with liver disease may require lower doses as risperidone is metabolized in the liver.
- Severity of Condition: Patients with more severe conditions may require higher doses than those with milder conditions.
Dosage Adjustment Based on Clinical Response
The initial dosage of risperidone is typically low and gradually increased until the desired therapeutic effect is achieved. The dosage should be adjusted based on the individual patient’s clinical response, with careful monitoring for adverse effects.
- Improved Symptoms: If the patient’s symptoms improve, the dosage may be maintained or reduced to the lowest effective dose.
- Unresponsive Symptoms: If the patient’s symptoms remain unresponsive to the current dosage, the dosage may be increased, but only after careful consideration of potential adverse effects.
- Adverse Effects: If the patient experiences significant adverse effects, the dosage may need to be reduced or the medication discontinued.
Practical Tips for Administering Risperidone
- Oral Administration: Risperidone tablets should be swallowed whole with water. They can be taken with or without food. The oral solution should be measured carefully using a calibrated dropper or syringe and administered directly into the mouth or mixed with a small amount of liquid.
- Injectable Administration: Injectable risperidone is administered intramuscularly or intravenously by a healthcare professional. It is essential to follow proper injection techniques and to monitor the patient for any adverse reactions.
- Monitoring: Regular monitoring of the patient’s clinical response, vital signs, and laboratory tests is crucial during risperidone therapy.
- Compliance: Encouraging patient compliance with the prescribed dosage and administration schedule is essential for achieving optimal therapeutic outcomes.
Monitoring and Management of Risperidone Therapy
Effective monitoring and management are crucial for optimizing risperidone treatment and minimizing potential risks. This involves regular assessments, proactive interventions, and ongoing adjustments to ensure the best possible outcomes for patients.
Monitoring Parameters
Regular monitoring of patients receiving risperidone is essential to identify and manage potential adverse effects, ensure therapeutic efficacy, and optimize treatment outcomes. Here are the key parameters to monitor:
- Clinical Response: Monitor for improvements in symptoms of psychosis, such as hallucinations, delusions, and disorganized thinking. Evaluate the patient’s overall mental state, including mood, behavior, and cognitive function.
- Extrapyramidal Symptoms (EPS): Regularly assess for signs of EPS, such as akathisia (restlessness), dystonia (muscle spasms), Parkinsonism (tremor, rigidity), and tardive dyskinesia (involuntary movements). Early detection and management of EPS are crucial to prevent long-term complications.
- Metabolic Parameters: Monitor for changes in weight, blood glucose levels, lipid profile (cholesterol and triglycerides), and prolactin levels. Risperidone can increase the risk of metabolic syndrome, which is a cluster of conditions that increase the risk of heart disease, stroke, and type 2 diabetes.
- Cardiovascular Health: Assess blood pressure and heart rate regularly. Risperidone can increase the risk of orthostatic hypotension (low blood pressure upon standing) and prolonged QT interval (a measure of the heart’s electrical activity), which can increase the risk of arrhythmias.
- Other Potential Side Effects: Monitor for other potential side effects, such as sedation, dizziness, dry mouth, constipation, blurred vision, and urinary retention.
Managing Potential Complications and Side Effects
Proactive management strategies are crucial to minimize the risks associated with risperidone therapy. Here are some key approaches:
- Early Detection and Intervention: Regular monitoring of the parameters discussed above allows for early detection of potential complications and side effects. This enables timely interventions to mitigate risks and prevent further complications.
- Dosage Adjustments: The dosage of risperidone may need to be adjusted based on the patient’s clinical response, tolerability, and monitoring results. In some cases, reducing the dosage or switching to a different antipsychotic medication may be necessary.
- Management of EPS: If EPS develop, treatment options include anticholinergic medications (e.g., benztropine, trihexyphenidyl) or beta-blockers (e.g., propranolol). In severe cases, a switch to a different antipsychotic with a lower risk of EPS may be considered.
- Metabolic Monitoring and Management: Lifestyle modifications, such as regular exercise, a healthy diet, and weight management, are essential for managing metabolic risks associated with risperidone. In some cases, medication adjustments or additional medications may be necessary to address specific metabolic concerns.
- Cardiovascular Monitoring and Management: Close monitoring of blood pressure and heart rate is essential. If orthostatic hypotension occurs, patients should be advised to rise slowly from a sitting or lying position. In cases of prolonged QT interval, the use of risperidone may need to be reevaluated.
- Symptom Management: For other side effects, such as sedation, dizziness, dry mouth, constipation, blurred vision, and urinary retention, symptomatic treatment and lifestyle modifications may be helpful.
Ongoing Evaluation and Adjustment of Risperidone Therapy
Risperidone therapy should be regularly evaluated and adjusted based on the patient’s clinical response, tolerability, and monitoring results.
- Regular Follow-up: Patients should have regular follow-up appointments with their healthcare provider to assess their progress, monitor for side effects, and adjust treatment as needed.
- Treatment Goals: The goals of risperidone therapy should be clearly defined and discussed with the patient. These goals may include symptom reduction, improvement in functioning, and overall well-being.
- Treatment Duration: The duration of risperidone therapy will vary depending on the individual patient and their specific needs. In some cases, long-term maintenance therapy may be necessary to prevent relapse.
- Discontinuation: Risperidone should not be abruptly discontinued, as this can lead to withdrawal symptoms. The dosage should be gradually reduced under the supervision of a healthcare provider.
Research and Development of Risperidone

Risperidone, a widely used atypical antipsychotic medication, continues to be a subject of ongoing research and development. Researchers are exploring its potential for treating various conditions beyond its initial indication for schizophrenia and bipolar disorder. Moreover, studies are examining its effectiveness in combination with other therapies and its impact on long-term outcomes.
Future Applications and Developments of Risperidone
Researchers are investigating the potential applications of risperidone in treating other conditions, such as:
- Tourette’s syndrome: Risperidone has shown promise in reducing tic frequency and severity in patients with Tourette’s syndrome, a neurological disorder characterized by involuntary movements and vocalizations.
- Autism spectrum disorder (ASD): Studies suggest that risperidone may help manage behavioral problems, such as aggression and self-injurious behaviors, in individuals with ASD.
- Post-traumatic stress disorder (PTSD): Preliminary research suggests that risperidone may be beneficial in treating PTSD, particularly in reducing nightmares and improving sleep quality.
- Irritable bowel syndrome (IBS): Some studies indicate that risperidone may alleviate symptoms of IBS, such as abdominal pain and diarrhea, by modulating gut motility and inflammation.
In addition to exploring new therapeutic applications, researchers are also working on developing novel formulations of risperidone, such as:
- Long-acting injectable formulations: These formulations provide sustained release of risperidone, reducing the need for frequent oral doses and improving adherence to medication.
- Transdermal patches: Transdermal patches offer a convenient and painless route of administration, potentially enhancing patient compliance.
Impact of Risperidone Research on Psychopharmacology
The research on risperidone has significantly impacted the field of psychopharmacology. It has:
- Advanced our understanding of antipsychotic mechanisms: Studies on risperidone have shed light on the complex neurobiological mechanisms underlying antipsychotic action, contributing to the development of more effective and targeted treatments for mental illnesses.
- Promoted the development of new antipsychotic medications: The success of risperidone in treating schizophrenia and bipolar disorder has inspired the development of other atypical antipsychotics with improved efficacy and tolerability profiles.
- Enhanced the understanding of the neurobiology of other disorders: Research exploring the potential applications of risperidone in treating conditions like Tourette’s syndrome, ASD, and PTSD has broadened our understanding of the neurobiological underpinnings of these disorders.
Risperidone in Different Populations
Risperidone’s use in different populations, particularly children, adolescents, pregnant women, breastfeeding mothers, and the elderly, requires careful consideration due to unique physiological and developmental factors.
Risperidone in Children and Adolescents
The use of risperidone in children and adolescents is primarily for the treatment of schizophrenia and bipolar disorder. However, it is important to note that the safety and efficacy of risperidone in this population have been established only for specific indications and age groups.
- Schizophrenia: Risperidone is approved for the treatment of schizophrenia in children and adolescents aged 13 to 17 years. It is typically used as a second-line treatment option after other antipsychotics have been tried.
- Bipolar Disorder: Risperidone is approved for the treatment of acute manic and mixed episodes associated with bipolar I disorder in children and adolescents aged 10 to 17 years. It is often used in combination with mood stabilizers.
The decision to prescribe risperidone to children and adolescents should be made after careful consideration of the potential risks and benefits. It is crucial to monitor for potential adverse effects, including metabolic changes, extrapyramidal symptoms, and tardive dyskinesia.
Risperidone in Pregnant Women and Breastfeeding Mothers
The use of risperidone during pregnancy and breastfeeding should be approached with caution due to the potential risks to the developing fetus and infant.
- Pregnancy: Risperidone crosses the placenta and may have adverse effects on the developing fetus. The potential risks include premature birth, low birth weight, and withdrawal symptoms in the newborn. In some cases, risperidone may be considered if the potential benefits outweigh the risks. However, it is important to weigh the risks and benefits carefully and to discuss the potential risks with the patient.
- Breastfeeding: Risperidone is excreted in breast milk and can be absorbed by the infant. The potential risks to the infant include sedation, extrapyramidal symptoms, and metabolic changes. If risperidone is necessary during breastfeeding, it is recommended to use the lowest effective dose and to monitor the infant closely for any adverse effects.
Risperidone in Elderly Patients
Elderly patients may be more susceptible to the adverse effects of risperidone, particularly those related to the central nervous system and cardiovascular system.
- Increased Risk of Adverse Effects: Elderly patients are at an increased risk of experiencing adverse effects such as falls, stroke, and death. This is because elderly patients are more likely to have underlying medical conditions that can be exacerbated by risperidone.
- Dosage Adjustments: Dosage adjustments may be necessary in elderly patients due to age-related changes in drug metabolism and clearance. It is important to start with a low dose and to monitor the patient closely for any adverse effects.
It is crucial to monitor elderly patients closely for any signs of adverse effects and to adjust the dosage as needed.
Patient Education and Counseling
This section provides information on risperidone therapy, including its purpose, potential benefits, and important considerations for patients. Understanding this information will help you make informed decisions about your treatment.
Patient Education Brochure
This brochure is designed to provide patients with essential information about risperidone therapy. It covers key aspects of the medication, including its purpose, how it works, potential benefits, and important safety considerations.
What is Risperidone?
Risperidone is a medication used to treat certain mental health conditions, including schizophrenia and bipolar disorder. It belongs to a class of drugs called atypical antipsychotics.
How Does Risperidone Work?
Risperidone works by helping to balance certain chemicals in the brain, known as neurotransmitters. These neurotransmitters play a role in mood, thinking, and behavior. By balancing these chemicals, risperidone can help to reduce symptoms of mental illness.
What are the Potential Benefits of Risperidone?
Risperidone can help to improve symptoms of mental illness, such as:
- Hallucinations
- Delusions
- Disorganized thinking
- Agitation
- Mood swings
It can also help to improve social functioning and quality of life.
Important Safety Considerations
- Side Effects: Like all medications, risperidone can cause side effects. Some common side effects include drowsiness, dizziness, weight gain, and movement problems. It is important to discuss any side effects you experience with your doctor.
- Drug Interactions: Risperidone can interact with other medications. It is important to tell your doctor about all the medications you are taking, including over-the-counter medications and herbal supplements.
- Pregnancy and Breastfeeding: Risperidone can be harmful to a developing fetus. It is important to discuss your treatment options with your doctor if you are pregnant or planning to become pregnant. Risperidone can also pass into breast milk and may harm a nursing infant. It is important to discuss your treatment options with your doctor if you are breastfeeding or planning to breastfeed.
- Alcohol: Avoid alcohol while taking risperidone, as it can increase the risk of side effects.
- Driving: Risperidone can cause drowsiness. Avoid driving or operating machinery until you know how this medication affects you.
Adherence to Treatment
It is important to take risperidone exactly as prescribed by your doctor. Do not stop taking risperidone without talking to your doctor, even if you feel better. Stopping risperidone abruptly can lead to withdrawal symptoms.
Monitoring and Follow-Up
Your doctor will monitor your progress while you are taking risperidone. This may involve regular appointments, blood tests, and other assessments. It is important to keep all appointments and to report any changes in your condition or any new symptoms you experience.
Counseling Script for Healthcare Professionals
This script provides a framework for healthcare professionals to discuss risperidone with patients. It covers key points to address, including the purpose of the medication, potential benefits, important safety considerations, and adherence to treatment.
Introduction
“Hello [patient’s name], I’m [your name], and I’m here to talk to you about risperidone. This medication has been prescribed to help manage your [mental health condition].”
Explanation of Risperidone
“Risperidone is an atypical antipsychotic medication. It works by helping to balance certain chemicals in your brain, known as neurotransmitters. These neurotransmitters play a role in mood, thinking, and behavior. By balancing these chemicals, risperidone can help to reduce symptoms of your mental illness.”
Potential Benefits
“Risperidone can help to improve symptoms of your mental illness, such as [list specific symptoms, e.g., hallucinations, delusions, disorganized thinking, agitation, mood swings]. It can also help to improve your social functioning and quality of life.”
Important Safety Considerations
“Like all medications, risperidone can cause side effects. Some common side effects include drowsiness, dizziness, weight gain, and movement problems. It is important to discuss any side effects you experience with me.
Risperidone can interact with other medications. It is important to tell me about all the medications you are taking, including over-the-counter medications and herbal supplements.
If you are pregnant or planning to become pregnant, it is important to discuss your treatment options with me. Risperidone can be harmful to a developing fetus.
If you are breastfeeding or planning to breastfeed, it is important to discuss your treatment options with me. Risperidone can pass into breast milk and may harm a nursing infant.
Avoid alcohol while taking risperidone, as it can increase the risk of side effects.
Risperidone can cause drowsiness. Avoid driving or operating machinery until you know how this medication affects you.”
Adherence to Treatment
“It is important to take risperidone exactly as I have prescribed. Do not stop taking risperidone without talking to me, even if you feel better. Stopping risperidone abruptly can lead to withdrawal symptoms.”
Monitoring and Follow-Up
“I will monitor your progress while you are taking risperidone. This may involve regular appointments, blood tests, and other assessments. It is important to keep all appointments and to report any changes in your condition or any new symptoms you experience.”
Questions and Concerns
“Do you have any questions or concerns about risperidone?”
Conclusion
“Thank you for your time. I hope this information has been helpful. Please feel free to contact me if you have any further questions or concerns.”
Ethical Considerations in Risperidone Use

Prescribing risperidone, like any other medication, comes with a set of ethical considerations that healthcare professionals must carefully navigate. It’s crucial to balance the potential benefits of treatment with the risks and ensure the patient’s autonomy and well-being are prioritized.
This section delves into the ethical implications of risperidone prescription, explores the potential for misuse and abuse, and offers recommendations for ethical decision-making in risperidone therapy.
Ethical Implications of Prescribing Risperidone
Prescribing risperidone involves ethical considerations related to informed consent, patient autonomy, and the potential for misuse and abuse. Healthcare providers must ensure that patients understand the risks and benefits of risperidone treatment, including potential side effects, and that they are fully informed before making a decision.
Informed consent is a cornerstone of ethical medical practice. It ensures that patients are fully aware of the potential risks, benefits, and alternatives to risperidone therapy. This includes discussing potential side effects, such as extrapyramidal symptoms (EPS), metabolic changes, and the risk of tardive dyskinesia.
Patient autonomy is another crucial ethical consideration. Patients have the right to make their own decisions about their healthcare, including whether or not to take risperidone. Healthcare providers should respect this autonomy and provide patients with the information they need to make informed choices.
Potential for Misuse and Abuse of Risperidone
Risperidone, like many other psychotropic medications, has the potential for misuse and abuse. This can occur when individuals use the medication for purposes other than those prescribed, such as to get high or to self-medicate. Risperidone can be abused for its sedative effects, particularly when used in combination with other substances, leading to potential health risks.
The potential for misuse and abuse is further amplified by the availability of risperidone on the black market. This can make it difficult to track the source of the medication and increase the risk of counterfeit or adulterated products.
Recommendations for Ethical Decision-Making in Risperidone Therapy
Ethical decision-making in risperidone therapy requires a careful balance between the potential benefits and risks of treatment.
Here are some recommendations for ethical decision-making in risperidone therapy:
- Obtain informed consent: Before initiating risperidone therapy, healthcare providers should engage in a thorough discussion with patients to ensure they understand the risks, benefits, and alternatives to treatment. This discussion should be tailored to the patient’s individual circumstances and comprehension level.
- Consider alternative treatments: Risperidone should not be the first-line treatment option unless other therapies have been ineffective. Healthcare providers should consider alternative treatments, such as psychotherapy or non-pharmacological interventions, before prescribing risperidone.
- Monitor for potential side effects: Patients should be closely monitored for potential side effects of risperidone, including EPS, metabolic changes, and tardive dyskinesia. Healthcare providers should adjust the dosage or consider alternative medications if necessary.
- Address concerns about misuse and abuse: Healthcare providers should be aware of the potential for misuse and abuse of risperidone and take steps to prevent it. This may include discussing the risks of misuse with patients and their families, carefully monitoring medication refills, and reporting suspected cases of misuse or abuse to the appropriate authorities.
- Promote patient autonomy: Healthcare providers should respect patient autonomy and allow patients to make their own decisions about their treatment. This includes providing patients with the information they need to make informed choices and supporting them in their decision-making process.
Historical Perspective of Risperidone
Risperidone, a potent antipsychotic medication, has played a significant role in revolutionizing the treatment of mental health disorders, particularly schizophrenia. Its development and approval were marked by groundbreaking research and clinical trials, leading to a profound impact on the lives of millions of individuals struggling with these conditions.
Development and Approval of Risperidone
Risperidone’s journey began in the 1980s at Janssen Pharmaceutica, a Belgian pharmaceutical company. The research team, led by Dr. Paul Janssen, aimed to develop a new generation of antipsychotics with improved efficacy and fewer side effects. Their efforts led to the synthesis of risperidone, a novel atypical antipsychotic.
The drug’s unique chemical structure and mechanism of action, targeting both dopamine and serotonin receptors, set it apart from traditional antipsychotics. Rigorous clinical trials conducted in the 1990s demonstrated risperidone’s effectiveness in treating positive and negative symptoms of schizophrenia, while also showing a reduced risk of extrapyramidal side effects.
In 1993, the United States Food and Drug Administration (FDA) approved risperidone for the treatment of schizophrenia. This marked a pivotal moment in the history of mental health care, providing clinicians with a new and effective tool to manage this debilitating disorder.
Impact of Risperidone on the Treatment of Mental Health Disorders
Risperidone’s introduction transformed the landscape of antipsychotic therapy, offering several advantages over conventional medications:
* Improved Efficacy: Risperidone demonstrated superior efficacy in treating both positive and negative symptoms of schizophrenia, including hallucinations, delusions, disorganized thinking, and social withdrawal.
* Reduced Extrapyramidal Side Effects: Atypical antipsychotics like risperidone exhibited a lower risk of extrapyramidal side effects, such as muscle stiffness, tremors, and involuntary movements, compared to traditional antipsychotics.
* Improved Quality of Life: The reduction in both positive and negative symptoms, along with fewer side effects, contributed to a significant improvement in the quality of life for individuals with schizophrenia.
* Broader Therapeutic Applications: Risperidone’s efficacy extended beyond schizophrenia, finding applications in the treatment of other mental health disorders, including bipolar disorder, Tourette’s syndrome, and aggression associated with dementia.
Key Milestones and Influential Figures
The development and approval of risperidone involved a collaborative effort by scientists, clinicians, and regulatory agencies. Several key milestones and influential figures played a crucial role in this process:
- 1980s: The synthesis of risperidone by Dr. Paul Janssen’s team at Janssen Pharmaceutica.
- 1990s: Extensive clinical trials demonstrating risperidone’s efficacy and safety profile in treating schizophrenia.
- 1993: FDA approval of risperidone for the treatment of schizophrenia.
- 1990s-Present: Continued research and development of risperidone, leading to the introduction of long-acting injectable formulations and expanded therapeutic applications.
“The development of risperidone marked a significant advance in the treatment of schizophrenia, providing a more effective and safer alternative to traditional antipsychotics.” – Dr. David S. Goldstein, psychiatrist and researcher
Risperidone has undoubtedly made significant strides in the treatment of mental health conditions, offering hope and relief to countless individuals. However, it is crucial to remember that this medication is not a cure-all. It is essential to approach risperidone therapy with a balanced understanding of its benefits and risks, always consulting with qualified healthcare professionals for proper diagnosis, treatment, and ongoing management. Through responsible use and ongoing research, risperidone continues to play a vital role in the journey towards mental well-being.
Risperidone is a medication often prescribed for conditions like schizophrenia and bipolar disorder. While it’s effective in managing these conditions, it’s important to understand its potential side effects. For instance, it can increase the risk of blood clots, which is why doctors may recommend a medication like effient for patients taking risperidone. Effient helps prevent blood clots, minimizing this particular risk associated with risperidone.